Feb. 01, 2019
At Mayo Clinic the foundational approach to complex medical problems has been a multidisciplinary collaborative approach, and this is certainly embraced in the setting of the adult congenital heart disease practice. In the current era, multimodality imaging techniques are being used more frequently as their utility is better appreciated.
There are several choices available when it comes to detailed imaging. Echocardiography has been the mainstay approach, has a long history in the practice and remains uniquely poised to delineate complex hemodynamic abnormalities noninvasively. Cardiac computerized tomography (CT) and magnetic resonance imaging (MRI) provide a good imaging alternative for patients in which echocardiography is problematic or inconclusive, which can be common in patients with multiple complex surgeries. Currently both cardiac CT and MRI are regarded as standard adjunctive imaging approaches to help with diagnosis, stratification of prognosis, surveillance for complications and as an alternative when standard echocardiography is inadequate.
Furthermore, as these techniques are becoming more mainstay in contemporary practice, the stance in the Mayo Clinic Adult Congenital Heart Clinic is to:
- Critically appraise their utility
- Help understand congenital heart disease and postoperative changes
- Approximate the clinical, surgical and imaging practices when it comes to planning future procedures for patients in need
Advanced imaging has been central to the continued advancement of the contemporary cardiovascular practice in the Adult Congenital Heart Clinic. "3D imaging provides a detailed understanding of the complex spatial relationships in the heart and vascular system that is required by cardiac surgeons, cardiologists, cardiac radiologists, and the cardiovascular device industry to successfully manage these complex diseases," says Nandan S. Anavekar, M.B., B.Ch., a cardiologist and imaging specialist at Mayo Clinic in Rochester, Minnesota. In congenital heart disease, the 3D relationships of cardiovascular structures can vary greatly from patient to patient and are often not immediately intuitive from 2D images. To address this dilemma, 3D printing of life-size, patient-specific models can help improve the understanding of cardiac and vascular anatomy.
تمدد الأوعية الدموية الكاذب في البطين الأيسر

تمدد الأوعية الدموية الكاذب في البطين الأيسر
(أ) يبين التصوير المقطعي المحوسب للقلب تمدد الأوعية الدموية الكاذب في البطين الأيسر (سهم عند الفم).
الصمام الأبهري البديل يعرض فتحة "قطع" القلب

الصمام الأبهري البديل يعرض فتحة "قطع" القلب
(ب) تبين الصورة المقابلة ثلاثية الأبعاد للصمام الأبهري البديل فتحة "قطع" القلب لعرض الحاجز والمظهر الجانبي لتجويف البطين الأيسر ومجرى تدفق الدم إلى الخارج.
مسبار يبين موقع وحجم فم مصاب بتمديد الأوعية الكاذب
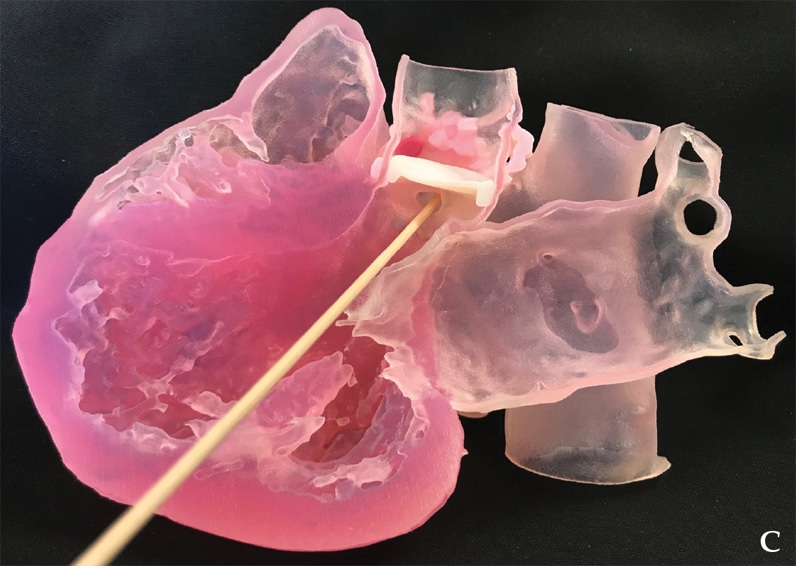
مسبار يبين موقع وحجم فم مصاب بتمديد الأوعية الكاذب
(ج) صورة مقابلة ثلاثية الأبعاد لصمام أبهري بديل تعرض المسبار يبين موقع وحجم فم مصاب بتمديد الأوعية الكاذب والعلاقة بالصمام الأبهري البديل (الهيكل الأبيض).
المظهر الخارجي للقلب وعلاقة تمدد الأوعية الدموية الكاذب بالشريان التاجي الأيمن
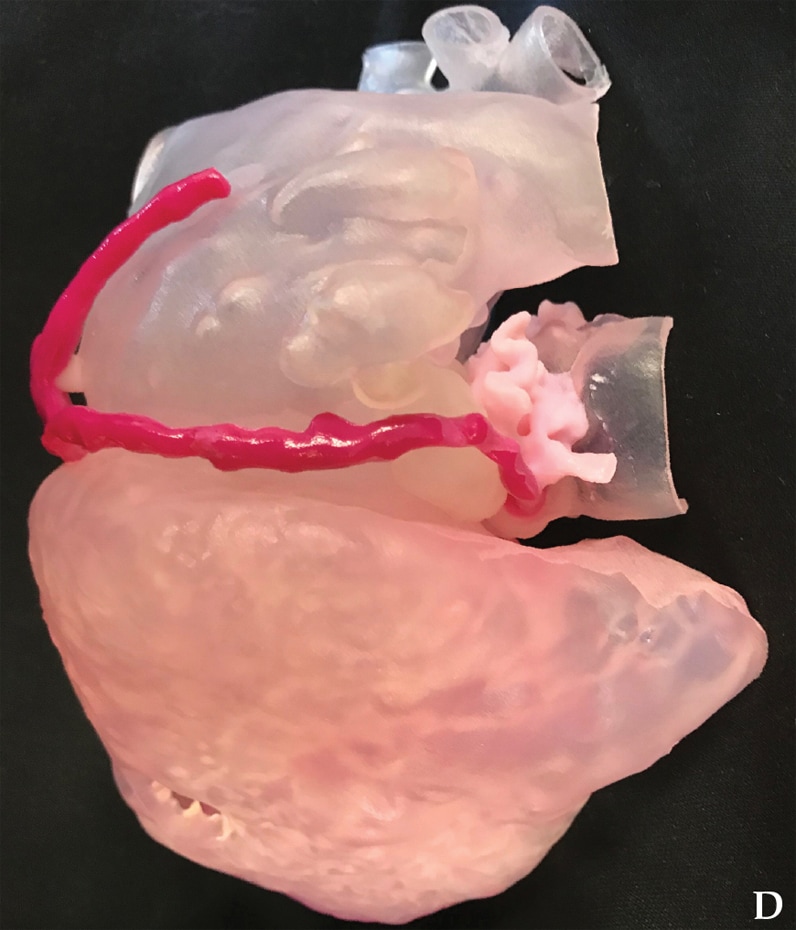
المظهر الخارجي للقلب وعلاقة تمدد الأوعية الدموية الكاذب بالشريان التاجي الأيمن
(د) صورة مقابلة ثلاثية الأبعاد لصمام أبهري بديل تعرض المظهر الخارجي للقلب وعلاقة تمدد الأوعية الدموية الكاذب (التشريح الشفاف) بالشريان التاجي الأيمن (التشريح باللون الأحمر).
الخصائص الداخلية للبطين والأذين الأيسر

الخصائص الداخلية للبطين والأذين الأيسر
(هـ) صورة ثلاثية الأبعاد مقابلة لصمام أبهري بديل تعرض الخصائص الداخلية للبطين والأذين الأيسر.
3D printing, an exciting, relatively new addition to the imaging armamentarium, is the process of creating a physical model based on a digital file using a 3D printer — a machine that lays down multiple layers of material guided by the model file. Medical 3D printing allows volumetric imaging data sets (most commonly CT, MRI or ultrasound images) to be converted into physical 3D replicas of anatomy. While this technology has been available since the early 1980s and has been used for planning dental and craniofacial surgery for over 25 years, 3D printing for cardiovascular applications has seen a significant growth only over the last several years. This technology not only shows promise as a cardiovascular diagnostic tool, but also has implications in therapies as 3D bioprinting may be useful for the creation of living 3D-printed implants.
Congenital heart defects are the most common type of birth defects, occurring in about 1 percent of all live births. A large number of these defects require surgery for management with a significant number, especially those in the category of complex congenital heart disease, requiring multiple operations. While there have been great advances in surgical technique and outcome, there still remains significant morbidity and mortality, especially in the setting of those requiring multiple operations. A major reason for this is the significant variation in anatomic abnormalities in patients with congenital heart disease, especially in those individuals requiring repeated procedures.
At the Mayo Clinic practice, 3D printing has seen a rapid growth in use for planning treatments for patients with congenital heart disease and carries hope in improving quality, efficiency and outcomes of these procedures. The current paradigm of the practice is to identify those individuals with complex anatomy who may require repeated procedures that carry significant risk. These individuals are discussed in a conference forum and all imaging materials are carefully reviewed ahead of time by cardiac imagers with specialization in congenital heart disease. With the advancement of 3D printing at the Mayo practice, life-size models using different materials can be held by the surgeon who can then immediately contemplate the approach and the technical feasibility of the anticipated procedure.
"The use of 3D-printed models can be used to tailor education to different learners," says Thomas A. Foley, M.D., a radiologist at Mayo Clinic in Rochester, Minnesota. "3D-printed models are being used to effectively teach complex cardiac anatomy to radiology, cardiology and cardiovascular surgery fellows." Training in procedural techniques has been traditionally time-consuming and has the potential to be implicated in procedural complications. Simulation using 3D models is emerging as a fundamental resource for teaching procedural techniques for trainees acquiring advanced skill sets in the field and is similarly being used within the Mayo Clinic practice as a new standard of care.
Finally, Mayo Clinic has found that 3D-printed models are also effective tools for communication within health care teams and with patients. Within the practice, specific 3D models used to explain disease processes and planned procedures enhance patient understanding and facilitate shared decision-making and informed consent, which ultimately improves patient satisfaction.
For more information
Mayo Clinic. Adult Congenital Heart Disease Clinic.