July 27, 2024
Findings of an epidemiological study published in the journal Maturitas surprised the Mayo Clinic authors. The study evaluated the frequency and type of premature and early menopause in a defined U.S. population for the 1988 to 2007 time period.
Two of the study's findings in young women were particularly unexpected by the investigators, says Walter A. Rocca, M.D., M.P.H., an epidemiologist at Mayo Clinic in Minnesota:
- Frequency of hysterectomy with ovarian conservation.
- Frequency of bilateral oophorectomy with or without concurrent hysterectomy.
The investigators found that 3.1% of women studied experienced premature (< age 40) spontaneous or induced menopause, and 6.2% experienced early (age 40 to 44) menopause.
"This is surprisingly high," says Dr. Rocca. "Approximately 1 in 10 women living in the general population have experienced premature or early menopause and are, therefore, at increased risk of morbidity and mortality."
Study rationale
Limited data regarding the frequency and type of premature and early menopause in women prompted Dr. Rocca, Ebbie A. Stewart, M.D., a gynecologist and reproductive endocrinologist at Mayo Clinic in Minnesota, and colleagues to investigate the topic. A significant reason for this lack of data, says Dr. Rocca, is that society considers menopause a normal fact of life, and the medical field has not given menopause adequate recognition. For example, details about age and type of menopause are often not collected in the medical record. Dr. Stewart compares menopause to puberty as a landmark in a woman's life span, yet with no medical classification.
Identifying the exact time of an individual's menopause is challenging even when the uterus is intact.
Medical documentation of women's cessation of menstruation is complicated by a fluctuating amenorrhea that many women experience as they approach menopause. If an individual has a hysterectomy conserving at least one ovary, the absence of menses makes identifying the cessation of ovarian function complex.
Study design and findings
مشتملات واستثناءات الدراسة
مشتملات واستثناءات الدراسة
هذا مخطط تفصيلي للمشتملات واستثناءات الدراسة.
جرت مراجعة السجلات الطبية لعدد 1653 امرأة مشمولة في الدراسة لتقييم حالة انقطاع الطمث حتى 31 ديسمبر 2021.
أُعيدت طباعة المخطط بإذن من Maturitas.
The Mayo Clinic investigators turned to the Rochester Epidemiology Project medical records linkage system, a unique Olmsted County, Minnesota, resource to study menopause in a geographically defined U.S. population.
Yet, even with this research infrastructure at their fingertips, identifying and evaluating the system's data was not a simple matter.
"The study required laborious and time-consuming manual abstraction of medical records by a physician," says Dr. Rocca.
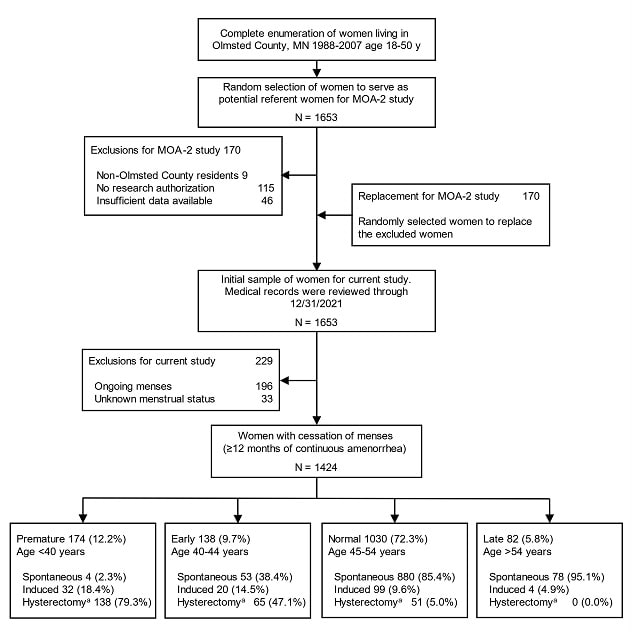
The study involved a random sampling of women ages 18 to 50 in Olmsted County, Minnesota, between the years of 1988 and 2007. The investigators noted the cessation of menstruation — defined as the spontaneous end of menses or the end of menses due to induced ovarian insufficiency — for each individual studied. They found that approximately 10% of women experienced spontaneous or induced premature or early menopause. Of this percentile, bilateral oophorectomy led to 78% of premature menopause and 23% of early menopause. Hysterectomy was the most frequent reason for the end of menstruation in women under age 40 (79%), and for women ages 40 to 44 (47%).
The rationale for bilateral oophorectomy performed during a hysterectomy did not relate to malignancy in most women studied: The women had an average cancer risk and were undergoing the surgery for generic ovarian cancer prevention, according to Dr. Rocca. In the U.S., only approximately 10% of hysterectomies are performed to treat a malignancy, according to an article published in Obstetrics and Gynecology.
Concern for elevated nonmalignancy-related hysterectomies and oophorectomies
According to Dr. Rocca, in past decades, the medical field's attitude has been that women risked no long-term negative consequences if they underwent hysterectomy or oophorectomy in the postreproductive phase of life. Thus, until 2005 to 2006, healthcare professionals did not question ovarian removal in women without ovarian conditions or in women with a benign ovarian condition.
"There was a thought in patients and some healthcare professionals that hysterectomy solved benign gynecologic conditions such as fibroids and prolapse, and that there were no downsides," says Dr. Stewart.
In fact, as the medical field now knows, women who have undergone hysterectomy even with ovarian conservation do face long-term sequelae. These include increased risk of anxiety, cardiac arrhythmia, coronary artery disease, depression, hyperlipidemia, hypertension and obesity. For bilateral oophorectomy, the range of long-term sequelae is even broader.
"Removing the uterus affects women's health," says Dr. Stewart, pointing to multiple studies suggesting long-term consequences of hysterectomy. "It's a large increase of risk and a large affected population. There are many reasons to be concerned."
However, Dr. Stewart notes that the medical field does not yet know a substantial amount about these sequalae over an individual's life span since most studies still have 20 years or fewer of follow-up, and most hysterectomies for benign disease are done for women in their 30s and 40s.
A call to rethink hysterectomy and oophorectomy
Dr. Stewart and Dr. Rocca advocate for women and their healthcare professionals to have a thorough discussion of all treatment options for a given gynecologic condition, reviewing risks and benefits of each.
"Unfortunately, many discussions prior to surgery just focus on hysterectomy's benefits," says Dr. Stewart. "A more robust shared decision-making process is needed."
The investigators urge women and their healthcare professionals to rethink hysterectomy or oophorectomy or both as options in the absence of malignancy, due to potential risks. Yet, they indicate the practice of automatically recommending these surgeries without presenting alternatives is still widespread. Dr. Stewart and Dr. Rocca encourage women and their healthcare professionals to review potential equally effective alternatives to hysterectomy and oophorectomy.
"In the absence of a cancer indication, all efforts should be made to conserve the uterus, the fallopian tubes and the ovaries," says Dr. Rocca. "Moreover, a recent study showed that in women with commercial insurance, where access to care should not be a problem, 60% had no medical or surgical options documented in the two years prior to hysterectomy," says Dr. Stewart.
The use of hysterectomy is legitimate when an individual is diagnosed with a gynecologic malignancy, or for the small percentage of women carrying a high-risk genetic variant predisposing them to ovarian cancer, says Dr. Stewart. In such cases, following a hysterectomy plus oophorectomy, the physician typically should prescribe estrogen replacement therapy to start promptly after surgery. Hysterectomy is also an option for women who have failed conservative therapies.
Dr. Stewart also encourages educating women for whom hysterectomy is an option.
"Education at the time of hysterectomy is important," she says. "Many women don't understand the separate roles of the uterus and ovaries, for example."
Dr. Stewart also believes informing female patients encourages them to become their own health advocates.
"Our study emphasizes the impact of gynecologic surgeries performed for noncancer indications on the menopausal status of women in a general population. Because both hysterectomy alone and bilateral oophorectomy have been linked to increased morbidity and mortality, the gynecologic practice should change radically."
At times, healthcare professionals do not offer hysterectomy alternatives. Dr. Stewart proposes potential reasons for a lack of options presented:
- Uninformed about new alternatives. Some hysterectomy alternatives, such as two recent FDA-approved uterine fibroid medications, are still new, and healthcare professionals may not have heard about them yet.
- Behind in following medical literature. The pandemic with its disruptions may have interfered with keeping up with the medical literature and findings of new options for patients.
- Uncertainty about alternatives requiring advanced training. Although every gynecologist is trained in performing hysterectomy, alternatives may require additional training.
Both Dr. Rocca and Dr. Stewart believe the medical field needs to reevaluate the use of hysterectomy and oophorectomy.
"Our study emphasizes the impact of gynecologic surgeries performed for noncancer indications on the menopausal status of women in a general population," says Dr. Rocca. "Because both hysterectomy alone and bilateral oophorectomy have been linked to increased morbidity and mortality, the gynecologic practice should change radically."
For more information
Wright JD, et al. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstetrics and Gynecology. 2013;122:233.
Rocca WA, et al. Frequency and type of premature or early menopause in a geographically defined American population. Maturitas. 2023;170:22.
Refer a patient to Mayo Clinic.