Oct. 08, 2021
A strategy highly customized to each patient is the best approach for endometriosis treatment, according to a Mayo Clinic multidisciplinary team specializing in the disease.
"During the past 10 to 20 years in gynecology, academic medicine taught hysterectomy plus removal of fallopian tubes and ovaries as a cure for endometriosis," says Tatnai L. Burnett, M.D., a minimally invasive gynecologic surgeon at Mayo Clinic's campus in Minnesota.
A qualitative approach
Dr. Burnett says that determining a treatment plan is not quite as simple as what's traditionally been taught. In fact, to decide the best plan for each patient with endometriosis, the surgeon must assess:
- The characteristics of the disease: superficial, deep or endometriomas
- Other concomitant diseases contributing to pain
- Previous medical and surgical treatments and their outcomes
- Fertility and other factors related to patient life stage and situation
"The plan to remove or not remove the patient's uterus should be personalized for what's best for the patient, specifically," says Dr. Burnett. "There is not a standard of care. It depends on how the uterus contributes to symptoms, and the woman's fertility and where she is in her life."
Dr. Burnett explains that patients with endometriosis may still find some surgeons who automatically tell them that the uterus and ovaries require removal. However, endometriosis specialists take a more nuanced approach using a combination of medications and surgery and addressing all pain sources, he says.
Rationale for a customized treatment approach is that endometriosis presents differently in different women. In addition, the following issues point to a need for a tailored approach:
- Hysterectomy plus ovary and fallopian tube removal doesn't cure 10% of affected patients.
- Patients with deep endometriosis may experience recurrence.
- Removal of both ovaries — especially for younger patients — may be detrimental for long-term health.
Treatment method and recurrence prevention
If a surgeon only removes the endometriosis, pain recurrence rates can be high: 50% recurrence in five years from original surgery. Dr. Burnett notes that to date, no investigator has produced a study demonstrating that excision alone produces vastly superior outcomes. "If I remove even the tiniest parts of endometriosis, we still see pain recurrence in some patients," says Dr. Burnett.
With removal of endometriosis plus the uterus, pain recurrence occurs in about 25% of cases. Dr. Burnett says recurrence rates decrease if the surgeon removes the uterus; yet whether the uterus itself is a pain generator is also central to the decision on its removal.
Often women diagnosed with endometriosis have greater pain sensitization, says Dr. Burnett, and many women who experience endometriosis have multiple causes of pain. "Pain syndromes tend to congregate, so pain is almost a disease in itself," he says.
Advanced treatment approach characteristics
Ideal specialized endometriosis therapy brings together all facets crucial to a patient's care, according to Dr. Burnett. While some medical centers excel in treating the whole patient with pain, or have strong fertility-related or imaging resources, he notes that Mayo Clinic is unique in having all these key pieces in place: experts in pain, reproductive endocrinology and women's health, plus high-quality imaging that can see even deep endometriosis.
Partnerships among surgical specialities also are important in care for this disease. Mayo Clinic gynecologic surgeons, for instance, routinely partner with colorectal and other specialty surgeons, working in tandem and sharing expertise in complex disease cases such as endometriosis that has spread to the bowel or ureter.
"The best way to treat endometriosis is to look at the whole patient and have a multimodal approach," says Dr. Burnett. "It's also important to be extremely precise removing endometriosis. When the decision to remove all disease is made, it's crucial to have the ability to do this even when it's on or near sensitive structures like the bowel or ureter."
Endometriosis
Endometriosis
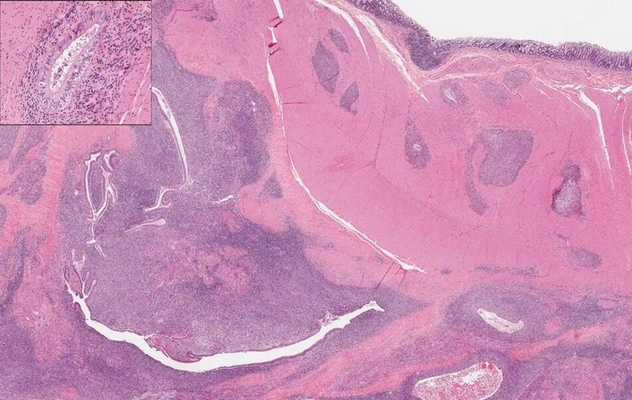
The uterine endometrium penetrates the intestinal wall. Inset: Endometrial gland.
Another key aspect of an advanced approach to endometriosis care is treating the disease while minimizing complications. This involves maximizing aggressive disease removal without damaging other organs or nerves, such as the uterosacral nerves. Dr. Burnett also explains a nuanced approach uses advanced imaging rather than diagnostic laparoscopic surgery — what he calls a "peek and shriek" — to observe the extent of disease, such as endometriosis impinging on the bowel. Dr. Burnett and colleagues explain the role of imaging versus diagnostic surgery in a January 10, 2020, article published in Abdominal Radiology.
Dr. Burnett says it's also crucial not to end endometriosis care after surgery. He and Mayo Clinic colleagues, for instance, bring patients back postsurgically to assess full treatment of symptoms and continued treatment of other pain generators. They also address postsurgical hormone treatment and therapy for sexual dysfunction.
"We're moving from hysterectomy with oophorectomy toward individualized care as the answer for women with endometriosis," says Dr. Burnett. "This kind of care is driven by an informed patient decision-maker. It combines preoperative diagnosis, aggressive disease removal when indicated and unaffected organ conservation. At the same time, addressing this disease involves treating all other causes of pain. With these shifts in approach, we have an opportunity to help our patients even more."
For more information
Burnett TL, et al. The role of imaging as a guide to the surgical treatment of endometriosis. Abdominal Radiology. 2020;45:1840.
Refer a patient to Mayo Clinic.