Jan. 09, 2024
 Endometriosis
Endometriosis
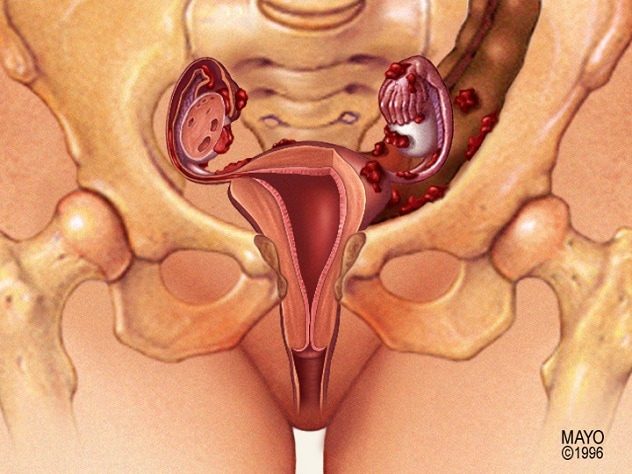
An anterior view of the uterus reveals endometriosis.
Despite undertaking mainstay treatment for endometriosis, at least 16% of patients experience persistent or recurring pain, says Isabel C. Green, M.D., a minimally invasive gynecologic surgeon at Mayo Clinic in Rochester, Minnesota.
"It's very frustrating for patients," she says. "They undergo treatment — sometimes 2 to 3 invasive surgeries they hope will resolve their pain. Yet these women experience recurrent pain."
Dr. Green indicates that this outcome can be especially disappointing because one or more surgeries to excise endometriosis can be costly in terms of time, finances, missed work and emotional stress. She is passionate about getting to the bottom of persistent pain after endometriosis surgery, optimizing the care around surgery to address the causes of patients' pain and identifying patients who may not benefit from surgery.
"What we'd like our surgical colleagues to move toward is not just surgical technique in excising endometriosis but looking deeper for other potential causes of pain. This is a different perspective on looking at a patient with endometriosis. It involves a switch from a surgical consult to a more general evaluation of pelvic pain and systems."
A fresh look at lingering pelvic pain
A review published by Dr. Green and colleagues in the December 2022 issue of Clinical Obstetrics and Gynecology recommends an expansion of pelvic pain evaluation and treatment by all healthcare professionals to stem unneeded surgery and address patients' needs.
"We're trying to look at our patients holistically," she says. "Quite often, a host of different conditions impacts a patient's pain. Management of this pain may not be straightforward; it may involve navigating an array of complex conditions or pain generators."
Dr. Green suggests considering the following steps as a start toward managing patients' persistent pain and improving quality of life:
- Past treatment. This involves contemplating whether surgery and medical treatment were optimized for the patient. One problem Dr. Green has noted frequently in reviews of patients' past surgeries is incomplete endometriosis excision.
- Multiple endometriosis phenotypes. Dr. Green indicates that there are different phenotypes of endometriosis and corresponding ways in which they affect individual patients.
-
Other possible contributors. Dr. Green and team also emphasize that there may be other contributing factors to a patients' pain, including other medical conditions, and these ideally should be discovered before proceeding to surgery.
"If comorbidities are unevaluated, a patient can have multiple surgeries hoping for a different outcome, but it's not going to happen," says Dr. Green. "The pain won't go away."
Specific pelvic pain factors to investigate beyond endometriosis
Assuming full excision of all visible endometriosis, other pain generators may come into play when a patient's pain persists. Examples include:
- Myofascial pain. Dr. Green encourages considering whether a patient may have myofascial pain, which she says can be discerned during surgical consult through listening to the patient's experience and examining the pelvic floor muscles and abdominal wall muscles.
- Psychological conditions. While Dr. Green is quick to state that lingering pelvic pain after endometriosis surgery is not ghost or psychological pain, a psychological condition can impact the sensation of pain. Mental health conditions impact how the nervous system manages and perceives pain.
-
Central sensitization syndrome. With this condition, central nervous system dysfunction can prompt pain to be caused by factors that should not create pain, explains Dr. Green. In some cases, components of a patient's central sensitization syndrome can dampen the effects of endometriosis excision and other treatment, she says. In fact, how the central nervous system and brain integrate endometriosis and central sensitization syndrome can be an essential component in a patient's pain.
Dr. Green says that endometriosis can cause harm beyond its immediate location and presence. This disease can interfere with a patient's nervous system plasticity, contributing to persistent pain once the endometriosis is treated or even pain in other parts of the body not directly impacted by endometriosis.
Assessment of patients with persistent pelvic
Patients with persistent pain after endometriosis surgery should see a larger healthcare team rather than one healthcare professional. This team should include specialists from gynecology, physical therapy, psychology and anesthesia. The team should collaborate with a patient's primary healthcare professional for optimal results. The initial visit should focus on full-body assessment to ascertain whether there are other factors influencing the patient's pelvic pain.
"What we'd like our surgical colleagues to move toward is not just surgical technique in excising endometriosis but also looking deeper for other potential causes of pain when a patient comes in for a surgical consultation," Dr. Green says. "This is a different perspective on looking at a patient with endometriosis. It involves a switch from a surgical consult to a more general evaluation of pelvic pain and multiple organ systems."
What Mayo Clinic offers for endometriosis
Dr. Green highlights the importance of identifying the right surgical team for women who have symptomatic endometriosis and need excisions or revisions.
At Mayo Clinic, surgeons who operate on endometriosis are fellowship trained and perform surgery for even the most complex endometriosis diagnoses. Mayo surgeons spend considerable time and training in preparation for managing these patients, handle a high volume of endometriosis surgeries and welcome patient referrals for consult.
"Ultimately, we want these patients to be able to do everyday activities, improve their quality of life and have a day uninterrupted by severe pain," says Dr. Green.
For more information
Green IC, et al. Persistent pelvic pain in patients with endometriosis. Clinical Obstetrics and Gynecology. 2022;65:775.
Refer a patient to Mayo Clinic.