June 21, 2022
A Mayo Clinic study of frozen donor egg in vitro fertilization (IVF) cycles published in a 2022 issue of Reproductive Sciences compared use of quality fresh versus frozen ejaculated sperm for intracytoplasmic sperm injection (ICSI). The results showed no statistically significant difference in live birth rate (LBR), the study's primary outcome, with 61.5% versus 52.6% LBR, respectively. The investigators examined use of 26 fresh sperm samples and 19 frozen sperm samples, with no significant intergroup demographic differences. Yet investigators propose that the absolute difference in live birth rates, 8.9%, could be clinically significant.
In vitro fertilization of egg with needle. IVF macro concept

In vitro fertilization of egg with needle. IVF macro concept
In vitro fertilization of egg with needle. IVF macro concept.
Frozen donor egg IVF cases are different from typical IVF because the couple is not present in the clinic on the day of egg thaw to conveniently provide a fresh sperm sample. This fresh sperm collection requires an extra appointment.
"We wanted to ask, 'When we could do either — fresh or frozen sperm — is fresh really better?' " says Chandra C. Shenoy, M.D., a reproductive endocrinologist at Mayo Clinic in Minnesota. "In both groups, cumulative pregnancy rate was over 55%; the LBR was over 50%. This reassures us that frozen sample use may be an alternative to fresh. However, fresh sperm ultimately may be a slightly better option if it is convenient."
Dr. Shenoy and fellow investigator Yulian Zhao, M.D., Ph.D., a reproductive endocrinologist at Mayo Clinic in Minnesota, indicate that they also found no statistically significant differences in secondary study outcomes — fertilization rate, blastocyst development rate and clinical pregnancy rate — between cohorts.
Although the difference in LBR was not statistically significant, the absolute difference was 8.9%, favoring fresh sperm. "If this difference were confirmed with a larger sample size, it would be statistically significant," says Dr. Shenoy, explaining that this would require approximately 650 sperm samples and take years for a single-institution study; a multisite study would be more feasible and may be warranted with this study's findings.
Drs. Shenoy and Zhao say clinicians and patients will be interested in these findings, as the use of fresh versus frozen sperm for ICSI has been an ongoing question for both groups, and 14% of the reproductive-age U.S. population experiences infertility.
Though over 95% of Mayo Clinic patients receiving ICSI use fresh sperm, this study's results are clinically important due to widespread use of frozen semen and increasing frozen donor oocyte use nationwide.
Study methodology
Intracytoplasmic sperm injection (ICSI)
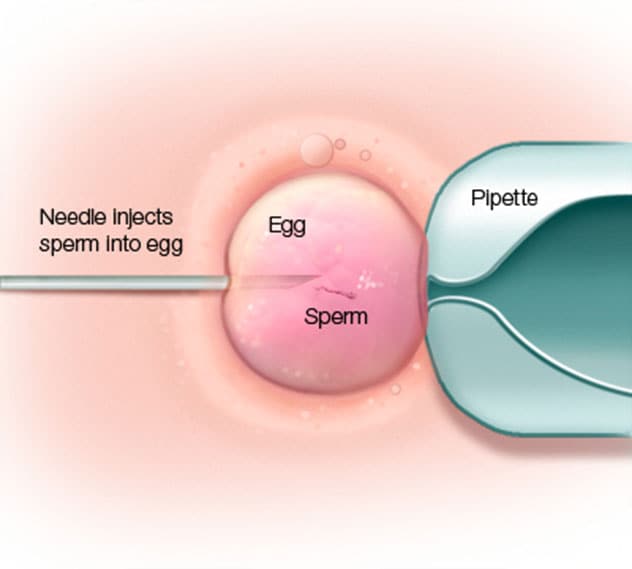
Intracytoplasmic sperm injection (ICSI)
Intracytoplasmic sperm injection (ICSI).
The investigators identified patients who initiated IVF with ICSI using frozen egg bank donor oocytes and fresh or frozen sperm. The researchers used two-sample t-tests and chi-square tests to compare outcomes, patient characteristics and sperm parameters. Of 45 cases studied, they observed no differences in average sperm morphology, egg bank utilized, infertility diagnosis, mean patient age or partner age at collection, or in median semen total mobile sperm count.
"Since we wanted to measure fresh versus frozen sperm use, the baseline involved the use of good sperm and good oocytes to minimize influence of variables," says Dr. Zhao. "Though you can't see DNA changes with your eyeball, you can tell visibly which are viable sperm by motility and morphology."
Concerns regarding frozen sperm for IVF with ICSI
To date, the reproductive endocrinology community's concerns about use of frozen ejaculated sperm rather than fresh have included the following, per the investigators:
- Cryopreservation effects on sperm quality and IVF outcomes
- Impaired fertilization capacity and sperm morphology, motility and survival reduction post-thawing
- Higher DNA fragmentation rates, linked to decreased live birth rates, arrested embryos and spontaneous abortion risk
Benefits of frozen sperm use for IVF with ICSI
The potential for effective frozen sperm use — with capacity for thawing, storage or transportation at any time — would have multiple benefits for patients and clinicians in the following scenarios, per the investigators:
- Allows for a backup sperm option, or to put someone giving a fresh sample more at ease due to its availability
- Provides an option when the sperm-providing partner is not present, such as a deployed partner or one unable to secure time away from work during the clinical workday
- Inability for the parents to be present at the medical center simultaneously — or preference for this arrangement — due to concerns such as child care or work schedules
- Preference to avoid an additional appointment to provide fresh sperm, especially if the couple lives far from the IVF center
- Preparation for future use, such as a young patient preparing for gonadotoxic cancer treatments
- Need for frozen donor sperm samples
- Convenient use of cryogenically preserved testicular sperm extraction, used in severe male factor infertility cases
Dr. Shenoy states that these findings underline the ability to use frozen sperm samples and thus support a complicated aspect of IVF: involving outside parties in family-building. Many donations arrive frozen.
Insights on the findings for referring physicians
Though this study may be broadly categorized as male IVF factor research, Dr. Shenoy indicates that it fits more precisely into the study of how to use embryos most effectively and notes that use of best possible sperm is crucial in this process.
"IVF is expensive and emotionally taxing, so you want to perform it in the best possible way," she says. "There's a lot of hope in these treatments."
To the investigators' knowledge, this is the first published study to examine outcome differences between fresh versus frozen ejaculated sperm samples in frozen donor oocyte IVF cycles with ICSI. They consider these findings important for allowing clinicians to confidently use frozen sperm in this procedure.
"I would tell physicians it would be fine to use frozen sperm or purchase frozen sperm from a sperm bank," says Dr. Zhao. "Fresh sperm may be slightly in favor, but frozen still has reasonable rates in all aspects."
Dr. Shenoy also suggests that fertility clinics evaluate how significant a stress it is on the individuals involved to travel to the clinic to give a fresh sperm sample.
"If logistically possible, do fresh," she says. "If you live far away, or an extra trip is a strain, it's OK to do frozen."
How Mayo Clinic can partner with external physicians in IVF
Mayo Clinic serves as a tertiary IVF care center, working with couples desiring to conceive from all over the United States. Dr. Zhao recommends referring patients to Mayo Clinic Reproductive Endocrinology and Infertility for IVF services any time there is an infertility concern, such as after 12 months attempting conception without pregnancy, if less invasive treatments or IVF has been unsuccessful.
"Often patients are tired when they first meet us in the fertility clinic, having tried alone or undergone procedures for some time," says Dr. Shenoy. "We try to offer them hope."
Dr. Shenoy also suggests referring patients quickly if time is limited, such as when women are age 35 or older and egg quality and quantity start to decrease.
Though some centers must turn away patients with certain risk factors — such as fibroids, obesity, endometriosis or advanced reproductive age — the Mayo Clinic practice works with these types of complex IVF scenarios. The IVF practice is high quality with many tools available, comprehensive and very patient-focused, say Drs. Shenoy and Zhao, noting that Mayo Clinic's IVF results are available on the Society for Assisted Reproductive Endocrinology website.
For more information
Miller CM, et al. Outcomes of frozen donor in vitro fertilization (IVF) cycles using fresh versus frozen sperm. Reproductive Sciences. 2022;29:1226.
Society for Assisted Reproductive Endocrinology.
Refer a patient to Mayo Clinic.