July 27, 2024
 In vitro fertilization
In vitro fertilization
In vitro fertilization of egg with needle.
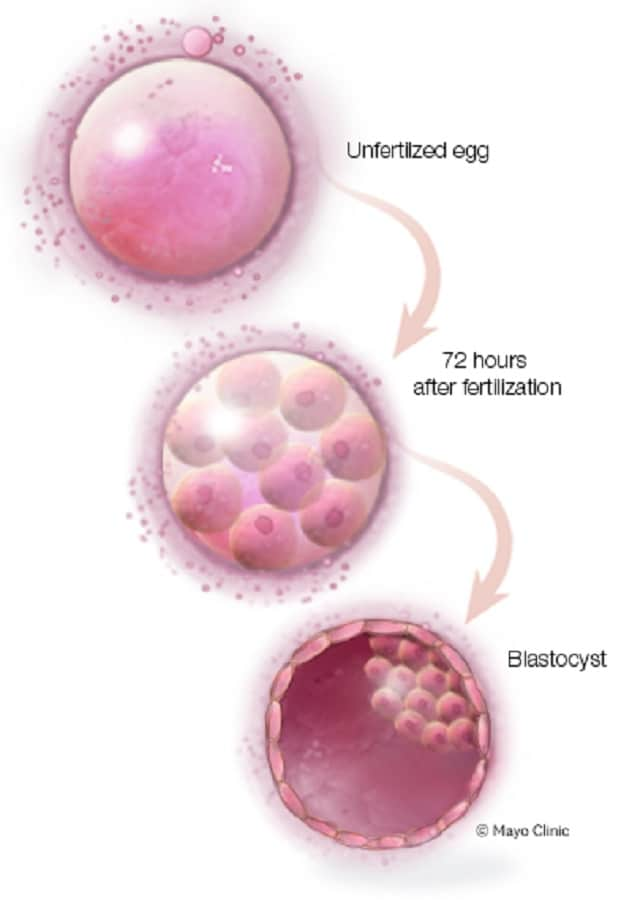 Blastocyst
Blastocyst
By the fifth day after fertilization, a fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. Blastomeres can be excluded from the blastocyst.
Mayo Clinic reproductive endocrinologists have discovered a new clue in the search for patterns to identify the best embryos for in vitro fertilization (IVF) transfer, detailed in a Reproductive Sciences publication. They discovered an association between blastomeres excluded late in the embryo development process and higher risk of aneuploid embryo genetics, which leads to poorer embryo health. In contrast, they found earlier blastomere exclusion indicated potential for embryo health and successful transfer.
"I don't know why embryos exclude cells, but I suspect they are trying to correct for abnormal genetics," says Chandra C. Shenoy, M.D., a reproductive endocrinologist at Mayo Clinic in Minnesota.
The investigators' findings represent one factor that can help embryologists using time-lapse incubators to monitor and pinpoint healthy embryos to select for transfer. The ability to distinguish healthy embryos especially benefits embryologists' selection processes where the parents have opted out of preimplantation genetic testing, which reveals abnormal chromosomes. If embryologists transfer unhealthy embryos, the abnormal genetics can lead to less successful transfers, a failed round of IVF or a miscarriage. On the other hand, if embryologists can identify and transfer healthy embryos, the likelihood of implantation and a healthy baby increase.
"This is one factor that can play into embryologists' decision-making on which embryos to favor for transfer," says Dr. Shenoy. "If they can do optimal, noninvasive embryo selection, it would prioritize a healthy pregnancy and singles versus multiples in each pregnancy. With more insight into healthier embryos to transfer, it reduces the need to perform more transfers and lessens pressure to transfer multiple embryos."
Though some families undergoing IVF request multiples, Dr. Shenoy says that singleton pregnancies have lower health risks for the mother and the baby than pregnancies with multiples. Thus, reproductive endocrinologists favor a healthy, singleton pregnancy, she says.
Study details and recommendations
In this retrospective cohort study, the Mayo Clinic investigators assessed blastomere exclusion and its relationship to embryo ploidy. The aneuploidy rate was 52.9% when no blastomere exclusion occurred and 68.5% for embryos that had evidence of blastomere exclusion at any point in the embryonic development. The investigators did not find a significant association with increased risk of aneuploidy with blastomere exclusion early in embryonic development.
The investigators discovered, however, that for blastomere exclusion occurring late in the embryonic development, the risk of aneuploidy was significantly higher (77.5%) compared with the embryos with no blastomere exclusion (52.9%). Embryos with early plus late blastomere exclusion also carried a higher risk of aneuploidy (71.2%) compared with embryos without blastomere exclusion (52.9%).
Additionally, the investigators found that blastomere exclusion trended toward a higher rate of complex aneuploidy (two more chromosomal abnormalities), as follows:
- With no blastomere exclusion, 38.7% of abnormalities were complex.
- With early blastomere exclusion, 37% of abnormalities were complex.
- With late blastomere exclusion, 45.5% of abnormalities were complex.
- With early plus late blastomere exclusion, 50% of abnormalities were complex.
Dr. Shenoy recommends incorporating these findings for selection of the best quality, genetically untested embryos for transfer while using the time-lapse photography embryo monitoring method.
[This animation shows time-lapse photography of how the embryo monitoring method is used to transfer embryos. It plays without audio.]
Time-lapse photography embryo monitoring technology
Time-lapse photography embryo monitoring controls the temperature and atmosphere around embryos while taking photos of them every 12 seconds, says Dr. Shenoy. The technology, which Mayo Clinic has used in the clinical setting for 10 years, allows embryologists to receive up-to-date, real-time information about the incubated embryos and view more events as they occur. A computer analyzes these images, providing ample information about the embryos. The advantage of time-lapse monitoring over its predecessor, according to Dr. Shenoy, is that it does not require embryo removal from the incubator every couple of days, decreasing embryonic stress from incubator removal.
For more information
Shenoy CC, et al. Embryo blastomere exclusion identified in a time-lapse culture system is associated with embryo ploidy. Reproductive Sciences. 2023;30:1911.
Refer a patient to Mayo Clinic.