Stages of labor and birth: Baby, it's time!
Labor is a natural process. Here's what to expect during the stages of labor and birth — along with some tips to make labor more comfortable.
By Mayo Clinic Staff
Labor is a unique experience. For some people, it's over in a matter of hours or less. For others, a long labor may test the limits of physical and emotional stamina.
You won't know how labor and childbirth will unfold until it happens. But you can prepare by understanding the series of events that typically takes place during labor and delivery.
Stage 1: Early labor and active labor
Cervical effacement and dilation
Cervical effacement and dilation
Cervical effacement and dilation
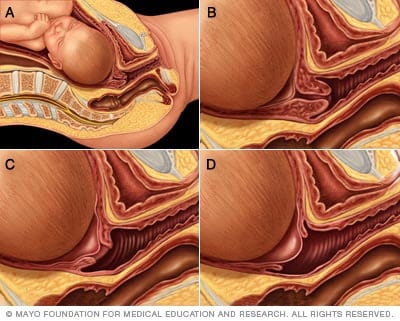
During the first stage of labor, the cervix opens. The medical term for this is dilation. The cervix also thins out. The medical term for this is effacement. Dilation and effacement usually happen together. This process allows the baby to move into the birth canal. In figures A and B, the cervix is tightly closed. In figure C, the cervix is 60% effaced and 1 to 2 cm dilated. In figure D, the cervix is 90% effaced and 4 to 5 cm dilated. The cervix must be 100% effaced and 10 cm dilated before a vaginal delivery.
The first stage of labor and birth happens when you begin to feel ongoing contractions. These contractions become stronger, and they happen more often as time goes on. They cause the cervix to open. This is called dilation. The contractions also soften, shorten and thin the cervix. That process is called effacement. It allows the baby to move into the birth canal.
The first stage of labor is the longest of the three stages. It's divided into two phases — early labor and active labor.
Early labor
During early labor, also called latent labor, the cervix opens and softens. It also gets shorter and thinner. The cervix opens less than 6 centimeters (cm) in early labor. Contractions tend to be mild, and they may not happen consistently.
As the cervix begins to open, you might notice a clear pink or slightly bloody discharge from your vagina. This likely is the mucus plug that blocks the cervical opening during pregnancy.
How long it lasts: Early labor isn't predictable. It may stop and start. The average length varies from hours to days. It's often shorter for people who have had a baby before.
What you can do: For many people, early labor isn't particularly uncomfortable. But contractions may be more intense for some. And sometimes contractions may continue for a long period of time during early labor. Try to stay relaxed.
The following may help keep you comfortable during early labor:
- Go for a walk.
- Take a shower or bath.
- Listen to relaxing music.
- Try breathing or relaxation techniques taught in childbirth class.
- Change positions.
If your pregnancy isn't high risk, you may spend most of your early labor at home. Most of the time, pregnant people don't need to go to a hospital or birthing center until contractions start to get more intense and happen more often. Talk to your healthcare professional about when to leave for the hospital or birthing center. If your water breaks or you have a lot of vaginal bleeding, contact your healthcare professional right away.
Active labor
During active labor, the cervix opens from 6 cm to 10 cm. Contractions become stronger and closer together. They also happen more consistently. Your legs might cramp. Your stomach may feel upset. If it didn't happen earlier, you might feel your water break. You also may feel more pressure in your back. If you haven't headed to your labor and delivery facility yet, now's the time.
Your initial excitement may fade as labor goes on and you get more uncomfortable. Ask for pain medication or anesthesia if you want it. Your healthcare team works with you to make the best choice for you and your baby. Remember, you're the only one who can judge your need for pain relief.
How long it lasts: Active labor often lasts 4 to 8 hours or more. On average, the cervix opens at approximately 1 cm an hour. But it may take longer for people who haven't had a baby before.
What you can do: Look to your labor partner and healthcare team for encouragement and support. Try breathing and relaxation techniques to ease pain. Use what you learned in childbirth class or ask your healthcare team for suggestions.
Unless you need to be in a specific position to allow for close monitoring of you and your baby, try the following to be more comfortable during active labor:
- Change positions.
- Roll on a large rubber ball (birthing ball).
- Take a warm shower or bath.
- Take a walk, stopping to breathe through contractions.
- Have a gentle massage between contractions.
If you need a Cesarean delivery, also called a C-section, having food in your stomach can lead to complications. If your healthcare professional thinks you might need a C-section, or if you have an epidural for pain relief, you may be limited to small amounts of clear liquids, such as water, ice chips, popsicles and juice, instead of solid foods.
The last part of active labor can be particularly intense and painful. Contractions come close together and can last 60 to 90 seconds. You may have pressure in your lower back and rectum. Tell a member of your healthcare team if you feel the urge to push.
If you want to push but your cervix isn't fully open, you'll likely need to wait. Pushing too soon could make you tired and cause your cervix to swell. That might delay delivery. Pant or blow through the contractions. This part of labor typically is short, lasting about 15 to 60 minutes.
Stage 2: The birth of your baby
It's time! You deliver your baby during the second stage of labor.
How long it lasts: It can take from a few minutes to a few hours to push your baby into the world. People who haven't had a baby before and those who have an epidural typically need longer to push compared to those who've had a baby or don't have an epidural.
What you can do: Push! Your healthcare professional asks you to bear down during each contraction or tells you when to push. Or you might be asked to push when you feel the urge to do so.
When it's time to push, you may experiment with different positions until you find one that feels best. You can push while squatting, sitting, kneeling — even on your hands and knees. A member of your healthcare team can check progress during pushing to help you know if your efforts are working.
At some point, you might be asked to push more gently — or not at all. Slowing down gives your vaginal tissues time to stretch rather than tear. To stay motivated, you might ask if you could feel the baby's head between your legs or see it in a mirror.
After your baby's head is delivered, the shoulders are delivered. Then the rest of the baby's body follows shortly. The baby's airway is cleared if necessary. If the delivery didn't involve any health concerns for you or your baby, your healthcare professional may wait a few seconds to a few minutes before the umbilical cord is cut. Waiting to clamp and cut the umbilical cord after delivery increases the flow of nutrient-rich blood from the cord and the placenta to the baby. This raises the baby's iron stores and lowers the risk of anemia. That helps with healthy development and growth.
Stage 3: Delivery of the placenta
After your baby is born, you'll likely feel a great sense of relief. You might hold the baby in your arms or on your belly. Cherish the moment. But there's still a little more to do. During the third stage of labor, you deliver the placenta.
How long it lasts: The placenta typically is delivered within 30 minutes.
What you can do: Relax! By now your focus has likely shifted to your baby. You might not be paying attention to what's going on around you. If you'd like, try breastfeeding your baby.
Mild, less painful contractions that are close together continue after delivery. The contractions help move the placenta into the birth canal. You push gently one more time to deliver the placenta. You might be given medicine before or after the placenta is delivered to encourage uterine contractions and minimize bleeding.
Your healthcare professional examines the placenta to make sure it's in one piece. If any pieces of the placenta are left in the uterus, they must be removed to prevent bleeding and infection. If you're interested, ask to see the placenta.
After you deliver the placenta, your uterus continues to contract to help it return to its usual size.
A member of your healthcare team may massage your belly. This helps the uterus contract to lessen bleeding.
Your healthcare professional checks to see whether you need repair of any tears of your vaginal area. If you didn't have an epidural, you'll receive an injection of local anesthetic in the area to be repaired.
Now what?
Savor this special time with your baby. Your preparation, pain and effort have paid off. Enjoy the miracle of birth.
July 23, 2024
- Funai EF, et al. Management of normal labor and delivery. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- Caughey AB, et al. Nonpharmacologic approaches to management of labor pain. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- Satin AJ. Labor: Diagnosis and management of the latent phase. https://www.uptodate.com/contents/search. Accessed Oct. 28, 2021.
- American College of Obstetricians and Gynecologists. Labor and delivery. In: Your Pregnancy and Childbirth: Month to Month. Kindle edition. 7th ed. American College of Obstetricians and Gynecologists; 2021. Accessed Oct. 28, 2021.
- Landon MB, et al. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. http://www.clinicalkey.com. Accessed Oct. 28, 2021.
- Meek JY, et al. The first feedings. In: The American Academy of Pediatrics New Mother's Guide to Breastfeeding. Kindle edition. 3rd ed. Bantam Books; 2017. Accessed Oct. 28, 2021.
- Cunningham FG, et al. Normal labor. In: Williams Obstetrics. 25th ed. McGraw-Hill Education; 2018. https://www.accessmedicine.mhmedical.com. Accessed Oct. 28, 2021.
- Larish AM (expert opinion). Mayo Clinic. Feb. 27, 2024.