June 19, 2015
Once considered rare, spontaneous intracranial hypotension (SIH) is now more commonly diagnosed and recognized as an important cause of headaches. SIH is typically the result of spontaneous cerebral spinal fluid (CSF) leak at the spine level; orthostatic headaches, low CSF pressure, and diffuse pachymeningeal enhancement on MRI are diagnostic hallmarks. However, SIH has a broad spectrum of clinical and imaging manifestations, and atypical cases are increasingly seen.
"The variability in just about every aspect of this disorder is substantial," says Bahram Mokri, M.D., an emeritus professor of neurology at Mayo Clinic in Rochester, Minnesota. "It can be difficult to diagnose and treat this syndrome."
Sophisticated imaging and experience with the vast clinical presentations of this disorder are keys to the diagnosis. When the source of the leak is accurately identified and if surgical repair is deemed the best management, complete and lasting relief of symptoms can be achieved. "The outcome can be dramatic for most of these patients," says David G. Piepgras, M.D., a consultant in Neurologic Surgery at Mayo Clinic in Rochester, Minnesota.
Spectrum of presentation
Mayo Clinic has been at the forefront of advances in SIH diagnosis and treatment. Over the past 25 years, Dr. Mokri and Dr. Piepgras have seen an estimated 700 patients with SIH. Articles summarizing many of the outcomes of Dr. Mokri's work were published in the May 2014 edition of Neurologic Clinics and September 2014 edition of Headache.
Initially, it wasn't uncommon for patients to be referred after misdiagnosis and treatment for conditions such as migraine or tension headache.
Based on work at Mayo Clinic, it now appears that the core pathogenic factor in SIH is decreased CSF volume rather than decreased CSF opening pressure. "Patients can have normal CSF pressure and yet have this syndrome," Dr. Mokri says. "MRI findings and clinical features seem to be variables that are dependent on the CSF volume."
Even orthostatic headache, the most common symptom of SIH, appears to vary. The time from change in the patient's posture from recumbent to standing and appearance of headache, or relief upon lying down — usually assumed to be a few minutes — can be much longer. The headache might be throbbing, but often is not, and pain can range from dull to severe. The headache is often but not always bilateral, and can be frontal, fronto-occipital, holocephalic or occipital.
Indeed, Dr. Mokri notes that not all patients with orthostatic headache have CSF leaks, and headaches related to CSF leaks are not all orthostatic: "Sometimes, orthostatic features may dampen, and the pain transform into a lingering, chronic daily headache."
The nonheadache manifestations of CSF leak also vary greatly, including but not limited to:
- Neck or interscapular pain
- Tinnitus, change in hearing and dizziness
- Nausea and emesis
- Gait unsteadiness
- Diplopia
- Trouble with memory or cognitive function
- Movement disorders, such as chorea or parkinsonism
A case series of movement disorders associated with spontaneous CSF leaks was published in the December 2014 issue of Cephalagia.
"Patients can be profoundly affected," Dr. Piepgras says. "The headache might be so disabling that the patient can't be up and working." He cites one patient seen at Mayo Clinic with a spinal CSF leak and brain sag so severe that a syrinx developed in the patient's spinal cord — which resolved after identification and repair of the leak.
Mujer con dolores de cabeza ortostáticos y dolor en la parte posterior del cuello y los músculos de los hombros
Mujer con dolores de cabeza ortostáticos y dolor en la parte posterior del cuello y los músculos de los hombros
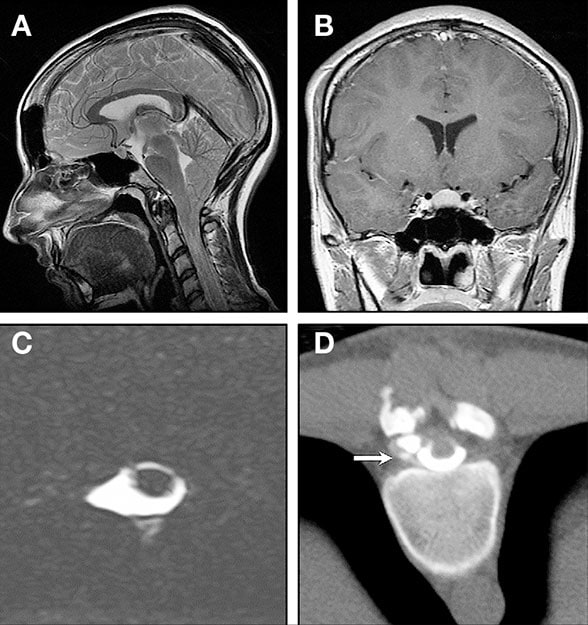
Diagnóstico por imágenes de una mujer de 23 años que desarrolló dolores de cabeza ortostáticos y dolor en la parte posterior del cuello y los músculos de los hombros. Tenía hipermovilidad articular y antecedentes familiares de hipermovilidad articular, pérdidas de líquido cefalorraquídeo y aneurismas aórticos y disección. El tratamiento para los dolores de cabeza por tensión no había sido eficaz. A. La vista sagital de la IRM de la cabeza muestra el descenso de las amígdalas cerebelosas, el aplanamiento de las protuberancias anteriores, la obliteración de la cisterna pre pontina y el atestamiento de la fosa posterior. B. Vista coronal de la IRM realzada con gadolinio que corta transversalmente la silla. Se puede observar el agrandamiento de la glándula pituitaria, la obliteración de la cisterna prequiasmática y la falta de realce paquimeníngeo anormal, que es poco común pero nada raro en las pérdidas de líquido cefalorraquídeo activas. C. La IRM de la columna (imagen axial intensamente ponderada en T2) muestra un divertículo meníngeo. D. La mielografía por tomografía computarizada hiperdinámica indica pérdidas en el divertículo meníngeo (flecha). Se extirpó quirúrgicamente, y el pequeño orificio de su conexión con la duramadre se suturó. Los dolores de cabeza finalizaron.
A significant minority of patients with SIH display clinical signs of heritable disorders of the connective tissue matrix. Although the etiology of spontaneous CSF leaks remains unknown in many patients, connective tissue weakness may play a role in the formation of meningeal diverticula and zones of dural weakness, resulting in CSF leaks.
Sealing CSF leaks
At Mayo Clinic, patients who haven't responded to initial conservative treatment — bed rest, hydration and time — are usually first treated with an epidural blood patch. Many require more than one patch. Although the overall success rate with each patch is about 30 percent, Dr. Mokri notes that, in his clinical experience, patients acknowledge the cumulative improvement when asked after several treatments to compare their symptoms with those before treatment started. Another treatment option is epidural injections of fibrin glue or blood and fibrin glue.
Surgery is considered if these less invasive treatments fail, and the source of the CSF leak is located. Mayo Clinic neuroradiologists have experience with CT myelogram and MRI with gadolinium contrast in these cases. Pinpointing a slow-flow leak remains a challenge; radioisotope cisternography can be helpful in providing evidence of slow-flow CSF leak but is less helpful in determining the precise site.
"The surgery itself may be difficult, particularly if the repair must be in front of the spinal cord, often in the thoracic area," Dr. Piepgras says. "But if you find the tear and stitch it up, the patient is cured."
Hombre con dolores de cabeza ortostáticos, mareos, náuseas e incontinencia de los intestinos y de la vejiga
Hombre con dolores de cabeza ortostáticos, mareos, náuseas e incontinencia de los intestinos y de la vejiga
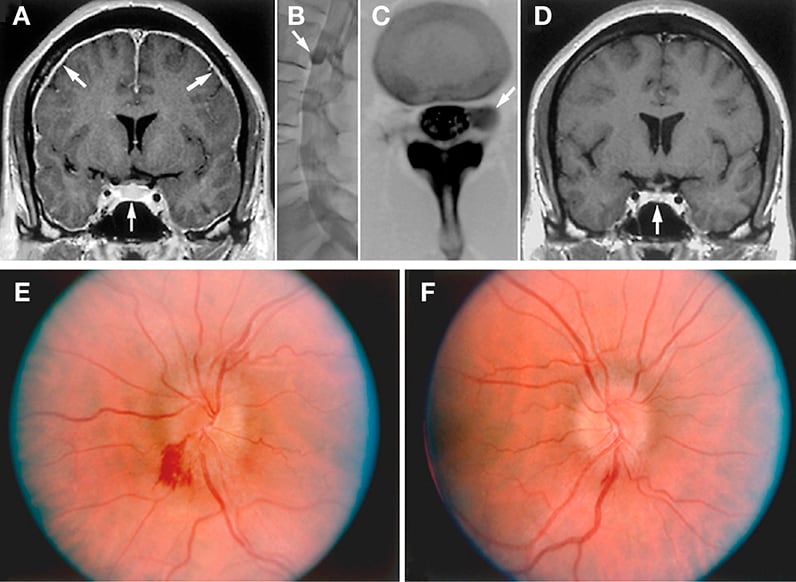
Diagnóstico por imágenes de un hombre de mediana edad que manifiesta dolores de cabeza ortostáticos, mareos, náuseas e incontinencia de los intestinos y de la vejiga. Hace diez años, se había sometido a una cirugía debido a una supuesta malformación de Chiari tipo I por haber manifestado síntomas similares pero sin una imagen por resonancia magnética (IRM) realzada. Los síntomas al principio disminuyeron, pero persistieron y después aumentaron. A. En la IRM de la cabeza se observa realce paquimeníngeo difuso (flechas superiores), agrandamiento de la glándula pituitaria (flecha inferior) y aplanamiento del quiasma óptico además del descenso de las amígdalas cerebelosas y cambios posoperatorios por la craniectomía suboccipital anterior y la laminectomía C1. B y C. La mielografía por tomografía computarizada muestra un divertículo meníngeo bastante grande (flechas) en el foramen neural L2 izquierdo, que se reparó quirúrgicamente. D. La flecha indica la reversión del agrandamiento de la glándula pituitaria y el aplanamiento del quiasma óptico después de la cirugía. Sin embargo, el paciente informó síntomas visuales imprecisos. E y F. Se detectó papiledema bilateral. La hipertensión intracraneal de rebote respondió favorablemente a la acetazolamida.
Successful treatment can sometimes result in rebound intracranial hypertension. Patients may re-present with headache that isn't necessarily orthostatic, and occasionally with papilledema. "The hypertension usually settles down in a matter of months," Dr. Mokri says. Acetazolamide may help ease symptoms.
Dr. Mokri notes that when he began practicing, a diagnosis of low CSF volume headache was largely unknown. Once MRI with contrast became available, he and Dr. Piepgras began seeing patients with diffuse meningeal enhancement and orthostatic headache often referred to Mayo Clinic with diagnoses such as chronic meningitis.
"But to me, it didn't make sense that fixed meningeal pathology would cause such an intermittent position-related headache," Dr. Mokri says. "And so we began researching and publishing."
For more information
Mokri B. Spontaneous CSF leaks: Low CSF volume syndromes. Neurologic Clinics. 2014;32:397.
Mokri B. Radioisotope cisternography in spontaneous CSF leaks: Interpretations and misinterpretations. Headache. 2014;54:1358.
Mokri B. Movement disorders associated with spontaneous CSF leaks: A case series. Cephalagia. 2014;34:1134.