June 19, 2015
Once considered rare, spontaneous intracranial hypotension (SIH) is now more commonly diagnosed and recognized as an important cause of headaches. SIH is typically the result of spontaneous cerebral spinal fluid (CSF) leak at the spine level; orthostatic headaches, low CSF pressure, and diffuse pachymeningeal enhancement on MRI are diagnostic hallmarks. However, SIH has a broad spectrum of clinical and imaging manifestations, and atypical cases are increasingly seen.
"The variability in just about every aspect of this disorder is substantial," says Bahram Mokri, M.D., an emeritus professor of neurology at Mayo Clinic in Rochester, Minnesota. "It can be difficult to diagnose and treat this syndrome."
Sophisticated imaging and experience with the vast clinical presentations of this disorder are keys to the diagnosis. When the source of the leak is accurately identified and if surgical repair is deemed the best management, complete and lasting relief of symptoms can be achieved. "The outcome can be dramatic for most of these patients," says David G. Piepgras, M.D., a consultant in Neurologic Surgery at Mayo Clinic in Rochester, Minnesota.
Spectrum of presentation
Mayo Clinic has been at the forefront of advances in SIH diagnosis and treatment. Over the past 25 years, Dr. Mokri and Dr. Piepgras have seen an estimated 700 patients with SIH. Articles summarizing many of the outcomes of Dr. Mokri's work were published in the May 2014 edition of Neurologic Clinics and September 2014 edition of Headache.
Initially, it wasn't uncommon for patients to be referred after misdiagnosis and treatment for conditions such as migraine or tension headache.
Based on work at Mayo Clinic, it now appears that the core pathogenic factor in SIH is decreased CSF volume rather than decreased CSF opening pressure. "Patients can have normal CSF pressure and yet have this syndrome," Dr. Mokri says. "MRI findings and clinical features seem to be variables that are dependent on the CSF volume."
Even orthostatic headache, the most common symptom of SIH, appears to vary. The time from change in the patient's posture from recumbent to standing and appearance of headache, or relief upon lying down — usually assumed to be a few minutes — can be much longer. The headache might be throbbing, but often is not, and pain can range from dull to severe. The headache is often but not always bilateral, and can be frontal, fronto-occipital, holocephalic or occipital.
Indeed, Dr. Mokri notes that not all patients with orthostatic headache have CSF leaks, and headaches related to CSF leaks are not all orthostatic: "Sometimes, orthostatic features may dampen, and the pain transform into a lingering, chronic daily headache."
The nonheadache manifestations of CSF leak also vary greatly, including but not limited to:
- Neck or interscapular pain
- Tinnitus, change in hearing and dizziness
- Nausea and emesis
- Gait unsteadiness
- Diplopia
- Trouble with memory or cognitive function
- Movement disorders, such as chorea or parkinsonism
A case series of movement disorders associated with spontaneous CSF leaks was published in the December 2014 issue of Cephalagia.
"Patients can be profoundly affected," Dr. Piepgras says. "The headache might be so disabling that the patient can't be up and working." He cites one patient seen at Mayo Clinic with a spinal CSF leak and brain sag so severe that a syrinx developed in the patient's spinal cord — which resolved after identification and repair of the leak.
直立性头痛及颈部后和肩部肌肉疼痛女性患者
直立性头痛及颈部后和肩部肌肉疼痛女性患者
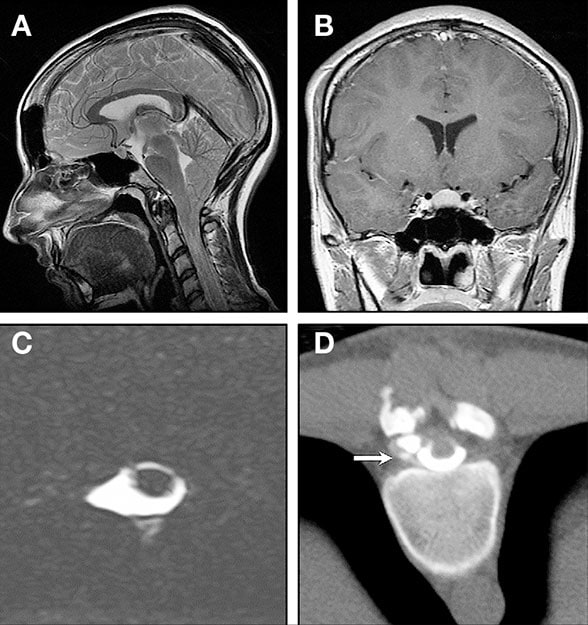
一位出现直立性头痛及颈部后和肩部肌肉疼痛的 23 岁女性的检查图像。她有关节过度活动综合征,而且有关节过度活动、脑脊液漏、主动脉瘤和主动脉夹层的家族病史。紧张性头痛的治疗方法无效。A. 头部 MRI 磁共振成像矢状位图显示,小脑扁桃体位置下移、脑桥腹侧变平、桥前池闭塞和颅后窝拥挤。B. 横切蝶鞍的钆增强 MRI 磁共振成像冠状位图。注意图中显示垂体增大、交叉前池闭塞——而且没有异常的硬脑膜强化,这属于异常,但在活跃的脑脊液漏中并不罕见。C. 脊柱 MRI 磁共振成像(轴向重 T2 加权图像)显示脑膜憩室。D. 高动态 CT 扫描脊髓造影显示脑膜憩室渗漏(箭头处)。手术将它切除,并缝合了与硬脑膜连接的小孔。头痛缓解。
A significant minority of patients with SIH display clinical signs of heritable disorders of the connective tissue matrix. Although the etiology of spontaneous CSF leaks remains unknown in many patients, connective tissue weakness may play a role in the formation of meningeal diverticula and zones of dural weakness, resulting in CSF leaks.
Sealing CSF leaks
At Mayo Clinic, patients who haven't responded to initial conservative treatment — bed rest, hydration and time — are usually first treated with an epidural blood patch. Many require more than one patch. Although the overall success rate with each patch is about 30 percent, Dr. Mokri notes that, in his clinical experience, patients acknowledge the cumulative improvement when asked after several treatments to compare their symptoms with those before treatment started. Another treatment option is epidural injections of fibrin glue or blood and fibrin glue.
Surgery is considered if these less invasive treatments fail, and the source of the CSF leak is located. Mayo Clinic neuroradiologists have experience with CT myelogram and MRI with gadolinium contrast in these cases. Pinpointing a slow-flow leak remains a challenge; radioisotope cisternography can be helpful in providing evidence of slow-flow CSF leak but is less helpful in determining the precise site.
"The surgery itself may be difficult, particularly if the repair must be in front of the spinal cord, often in the thoracic area," Dr. Piepgras says. "But if you find the tear and stitch it up, the patient is cured."
出现直立性头痛、头晕、恶心、大便失禁和膀胱失禁的男性患者
出现直立性头痛、头晕、恶心、大便失禁和膀胱失禁的男性患者
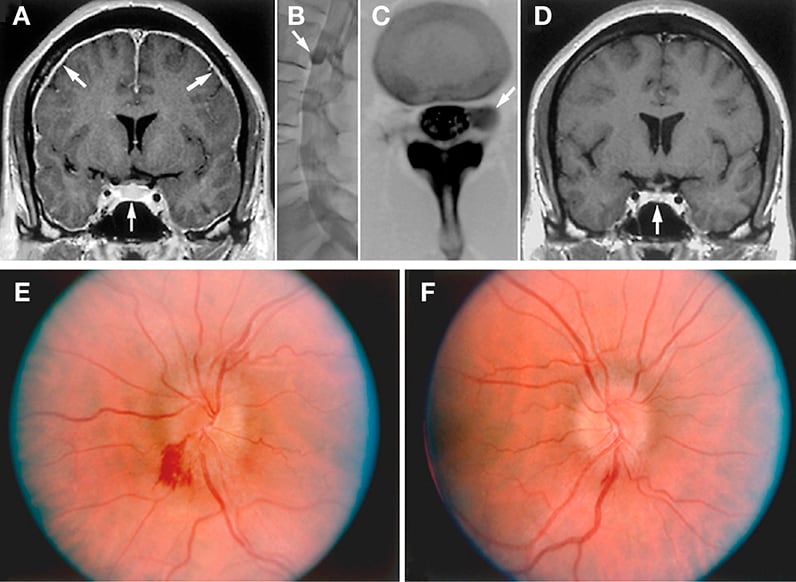
出现直立性头痛、头晕、恶心、大便失禁和膀胱失禁的中年男性患者的影像学检查。十年前,他因出现类似症状而被认为可能患有下疝畸形 I 型而接受了手术,当时没有进一步接受磁共振成像 (MRI) 检查。症状起初有所减轻但仍然在持续,随后加剧。A. 头部磁共振成像 (MRI) 显示除了出现小脑扁桃体下疝,以及此前接受枕下颅骨切除术和 C1 椎板切除术后的变化以外,还出现弥漫性硬脑膜强化(上箭头)、垂体增大(下箭头)和视交叉变平。B 和 C. CT 扫描脊髓造影显示左侧 L2 神经孔有极大的脑膜憩室(箭头处),而且已经过手术修复。D. 箭头指出手术后垂体增大和视交叉变平发生逆转。但是,患者报告称有视力模糊的症状。E 和 F. 发现双侧视神经乳头水肿。反弹性颅内高血压对乙酰唑胺反应良好。
Successful treatment can sometimes result in rebound intracranial hypertension. Patients may re-present with headache that isn't necessarily orthostatic, and occasionally with papilledema. "The hypertension usually settles down in a matter of months," Dr. Mokri says. Acetazolamide may help ease symptoms.
Dr. Mokri notes that when he began practicing, a diagnosis of low CSF volume headache was largely unknown. Once MRI with contrast became available, he and Dr. Piepgras began seeing patients with diffuse meningeal enhancement and orthostatic headache often referred to Mayo Clinic with diagnoses such as chronic meningitis.
"But to me, it didn't make sense that fixed meningeal pathology would cause such an intermittent position-related headache," Dr. Mokri says. "And so we began researching and publishing."
For more information
Mokri B. Spontaneous CSF leaks: Low CSF volume syndromes. Neurologic Clinics. 2014;32:397.
Mokri B. Radioisotope cisternography in spontaneous CSF leaks: Interpretations and misinterpretations. Headache. 2014;54:1358.
Mokri B. Movement disorders associated with spontaneous CSF leaks: A case series. Cephalagia. 2014;34:1134.