Feb. 16, 2021
As a high-volume center for spinal deformity care, Mayo Clinic has the expertise required to treat even the most challenging conditions. Orthopedic surgeons routinely work alongside neurosurgeons and other specialists to optimize outcomes and enhance patient safety in complex procedures such as vertebral column resection (VCR).
"The Mayo Clinic care model is designed to allow different subspecialties to work together to care for complicated patients. That has been a long-standing and successful strategy for great patient care," says Anthony A. Stans, M.D., a pediatric orthopedic surgeon and surgeon-in-chief of the Mayo Clinic Children's Center in Rochester, Minnesota.
وضع مسامير مباشرة على التصوير المقطعي المحوسب
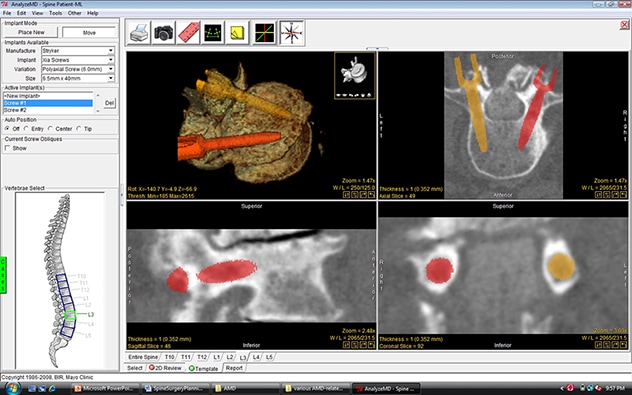
وضع مسامير مباشرة على التصوير المقطعي المحوسب
تتيح برمجيات مايو كلينك لجراحي العظام وضع المسامير مباشرةً على التصوير المقطعي المحوسب للمريض كجزء من التخطيط الجراحي.
This multidisciplinary approach to VCR and other complex spinal procedures incorporates extensive pre-surgical planning and the latest imaging technology. A high-resolution CT scan of the spine deformity is acquired. The image data is then exported into spinal surgery planning software developed by Mayo's Biomedical Imaging Resource Core and Paul M. Huddleston III, M.D., a Mayo orthopedic spinal surgeon. The software allows surgeons to analyze individual vertebrae and virtually place pedicle screw implants in the optimal position within each vertebra.
Mayo's 3D anatomic modeling laboratories export the surgical planning images to a 3D printer, which prints a life-size model with pedicle screw holes in optimal locations. A complete pre-surgical model can be created in just one to two days. "The model is very helpful on several levels," Dr. Stans says. "The process forces us to analyze every single vertebra and decide whether screws can be placed safely. Effectively performing pedicle screw placement on the computer in advance of the operation, and identifying the optimal starting point, trajectory and screw size, saves time and increases safety during surgery."
The 3D model is brought into the operating room and referred to during the procedure. Additional technology and expertise in the operating room help further ensure a successful outcome. Intraoperative spinal cord monitoring is performed by highly trained technicians and monitored by a neurophysiologist on-site. Anesthesiologists with special interest and expertise in spinal surgery use an anesthesia protocol to optimize the accuracy of spinal cord monitoring, minimize blood loss and maximize postoperative pain control. Intraoperative CT and computer navigation are used to guide the placement of pedicle screws.
All members of the patient care team have spinal deformity expertise, including nurses and anesthesiologists dedicated to caring for patients during complex spinal procedures. Postoperative care and rehabilitation are provided by physical medicine and rehabilitation specialists, pain specialists, and physical and occupational therapists who routinely work with people who have spinal deformity surgery.
"Our experience and collaboration across specialties allow us to treat all types of spinal deformities, in patients of all ages," Dr. Stans says. This technology and expertise help provide excellent outcomes for even the most challenging deformities."
صورة ثلاثية الأبعاد للعمود الفقري قبل الاستئصال

صورة ثلاثية الأبعاد للعمود الفقري قبل الاستئصال
صورة فوتوغرافية توضح تصويرًا ثلاثي أبعاد للعمود الفقري للمريض قبل استئصال الفقرات في مايو كلينك.
Dr. Stans cites a young woman whose severe scoliosis was corrected at Mayo Clinic. "With a curve this severe, she was becoming increasingly short of breath," he says. "She sang in her university choir but found she could no longer hold a long note very well."
Dr. Stans performed a VCR alongside Jeremy L. Fogelson, M.D., a Mayo Clinic neurosurgeon who has complementary expertise in complex spinal surgeries. The two surgeons routinely perform VCR together.
صورة إشعاعية مأخوذة قبل العملية توضح وجود جنف

صورة إشعاعية مأخوذة قبل العملية توضح وجود جنف
صورة إشعاعية مأخوذة قبل العملية توضح وجود جنف حاد.
صورة إشعاعية تالية للعملية توضح التصحيح

صورة إشعاعية تالية للعملية توضح التصحيح
صورة إشعاعية تالية للعملية الجراحية توضح تصحيحًا ممتازًا بعد استئصال العمود الفقري وأجهزة العمود الفقري الخلفية.
After surgery, the patient quickly found that she could fill her lungs. "Six months after surgery, she went on a 6-mile hike in the Cascade mountains," Dr. Stans says.
Several years before coming to Mayo Clinic, the patient had been seen elsewhere and advised to undergo corrective surgery. But she and her family were reluctant to proceed with the procedure recommended there, as it involved a thoracotomy, anterior release and partial vertebrectomy, followed by posterior instrumentation and fusion.
"At Mayo, we do VCR with one incision, as a staged procedure over two days," Dr. Stans says. "This strategy allows us to do the initial steps of the operation on the first day, and then perform the most challenging parts early on the subsequent day when the patient is in optimal medical condition and the surgical team is fresh and at the top of their game."
In the years before coming to Mayo Clinic, the patient's deformity had worsened. At the same time, her younger sister also developed severe scoliosis. The sister came to Mayo Clinic first and had scoliosis surgery. "After the younger sister's successful surgery, the older sister decided to go ahead with the VCR operation," Dr. Stans says. "At Mayo Clinic, the combination of advanced technology, specialized expertise and collaboration across medical specialties allows us to successfully and safely care for patients with complex spinal deformity."