Sept. 24, 2019
Wound complications are a major source of morbidity in patients undergoing radiation therapy and surgical resection for soft tissue sarcoma. Mayo Clinic is conducting a prospective clinical trial of intraoperative fluorescence angiography to evaluate whether it can reduce the risk of wound-healing complications in patients undergoing sarcoma reconstruction.
ساركومة شحمية مخاطية في الجزء الخلفي من الفخذ
ساركومة شحمية مخاطية في الجزء الخلفي من الفخذ
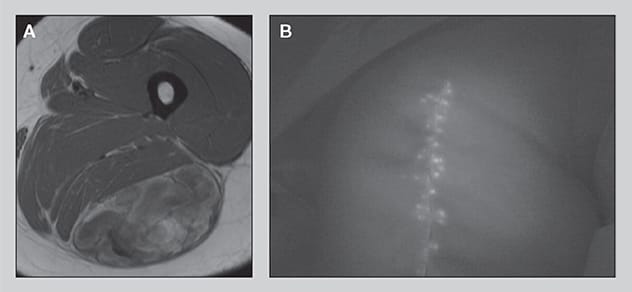
أ. ساركومة شحمية مخاطية في الجزء الخلفي من الفخذ لامرأة تبلغ من العمر 38 عامًا عُولِجَتْ في Mayo Clinic، وخضعت للعلاج بالإشعاع، ثم تلاه استئصال جراحي مع إغلاق مُركَّب. بعد الإغلاق الجراحي، أظهر التصوير الوعائي الفلوريسيني أثناء العملية تدفُّق دم ممتازًا إلى حوافِّ الجلد. ب. تَعَافَتِ المريضة مع عدم وجود مشكلات في الجرح بعد العملية الجراحية.
The clinical trial will compare the outcomes of sarcoma reconstructive surgery using a new fluorescence imaging device with outcomes for patients having the same surgery without fluorescence angiography. The device assesses blood flow and tissue perfusion after the intravenous administration of indocyanine green in patients undergoing surgery. Tissue that is identified as nonviable can be surgically removed.
"Historically, patients having this procedure have faced about a 35% chance of developing a wound complication. We hope that using this technology will significantly reduce that risk," says Courtney E. Sherman, M.D., an orthopedic surgeon at Mayo Clinic's campus in Florida.
Soft tissue sarcoma poses challenges throughout the process of diagnosis and treatment. The disease is rare — many orthopedic surgeons will see only one or two cases during their careers — and frequently misdiagnosed.
"Most sarcomas are painless. The masses are often noticed following an incidental trauma. The differential for soft tissue masses is large, but sarcoma must be considered," Dr. Sherman says. A delay in diagnosis can result in unnecessary amputation. In addition, the unplanned excision of a soft tissue sarcoma can result in high morbidity and possibly amputation. "If there is any doubt about the diagnosis, a biopsy is in order," Dr. Sherman says.
As a large tertiary center, Mayo Clinic has experience with the diagnosis and treatment of soft tissue sarcoma, including high-grade tumors. "We have a multidisciplinary approach. Our orthopedic surgeons, radiation oncologists, medical oncologists, radiologists and pathologists work as a team. That allows us to provide the complex management that these patients need, and the most up-to-date treatment options," Dr. Sherman says.
Mayo Clinic radiologists use ultrasound and advanced MRI imaging, including fat-suppression sequences and gadolinium enhancement, to aid the diagnosis of soft tissue sarcoma. The utility of this imaging for soft tissue sarcoma is highly technique dependent. Mayo Clinic surgeons also use the latest techniques, including minimally invasive surgery, limb-sparing surgery and intraoperative radiation therapy.
The prognosis for patients with soft tissue sarcoma depends on tumor type. Patients with low-grade tumors have a five-year survival rate of 90%; for patients with metastatic lesions, that rate is 15%. Through research and multidisciplinary diagnosis and treatment, Mayo Clinic is working to improve the management of soft tissue sarcoma.
"Our goal is to give our patients expertise from multiple specialties, to provide them with the optimal treatment options," Dr. Sherman says.