Jan. 16, 2024
"The glory of medicine is that it is constantly moving forward."
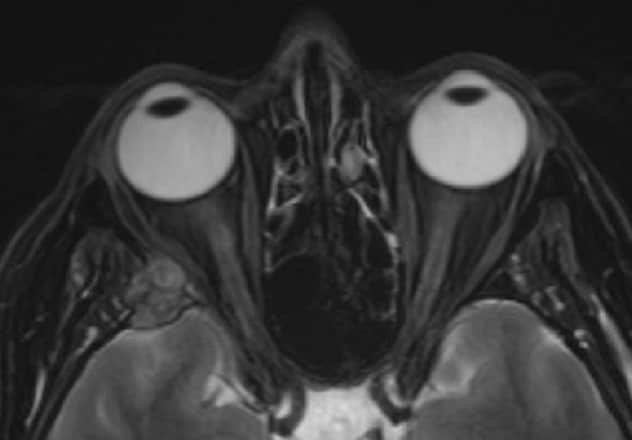 صورة تصوير بالرنين المغناطيسي
صورة تصوير بالرنين المغناطيسي
تُظهِر صورة تصوير بالرنين المغناطيسي ورمًا في الحفرة القحفية الوسطى الأمامية، يمتد إلى الحجاج الجانبي ويؤدي إلى إزاحة العضلة المستقيمة الجانبية. أُزيل هذا الورم خلال عملية جراحية مشتركة أجراها جراحو العيون وجراحو الأعصاب باستخدام طريق الحجاج مع شق ثنية الجفن.
Collaborating across clinical practice allows for discovery and quicker application of knowledge to develop new, patient-centered solutions. This approach has allowed Mayo Clinic ophthalmologists to work together with their colleagues across multiple specialties to offer the most promising surgical approaches for meningiomas of the skull base and improve patient outcomes.
Meningiomas account for 15% to 20% of primary brain tumors. A meningioma of the skull base is typically a noncancerous and slow-growing tumor that develops in the covering of the base of the brain. While mostly benign, these neoplasms can become aggressive and grow from the dura to extracranial spaces such as the orbit and nasal cavity. Many meningiomas are asymptomatic; however, when symptoms do present, they include headaches, anosmia and visual deficits that can significantly impact quality of life.
"The current standard treatment for patients with symptomatic anterior skull base meningiomas consists of unilateral frontal or bifrontal craniotomies," says Lilly H. Wagner, M.D., an oculoplastic and orbital surgeon at Mayo Clinic in Rochester, Minnesota. "While this approach has high rates of complete resection, it also carries a variety of risks including postoperative cerebral edema and visual morbidity due to manipulation of the optic nerve."
One alternative, the endoscopic endonasal approach (EEA), has been increasingly used, as it can provide better visualization of important vascular and nerve structures. It can also reduce operative time and eliminate the need for brain retraction, where appropriate. However, there are anatomical limitations, which make it challenging to reach lesions extending to lateral parts of the anterior skull base with EEA.
Minimally invasive supraorbital craniotomy has emerged as another option for anterior skull base meningioma resection in select patients. "Advantages of a supraorbital approach include the use of dynamic brain retraction, reduced risk of postoperative encephalomalacia, shorter length of time in the hospital and improved cosmetic results," says Dr. Wagner.
Existing literature predominantly focuses on the use of the supraorbital approach for small meningiomas, and it also carries its own risks. "The classic supraorbital keyhole approach creates a small craniotomy in the frontal bone," says Dr. Wagner. "Risks associated with this approach include unintentionally opening the frontal sinus, weakness of the frontal branch of the facial nerve and cosmetic deformity due to burr holes.
"Unfortunately, the supraorbital approach does not provide access to intraorbital tumor components," continues Dr. Wagner. "And there remains a gap in knowledge surrounding the role of oculoplastic surgeons in the management of such cases."
With recent advances — and the close collaboration among experts in ophthalmology, neurology and otolaryngology — transorbital neuroendoscopic surgery provides access to the skull base through the orbit and can provide sufficient exposure for total resection while avoiding the complications of traditional supraorbital keyhole craniotomy.
"Traditional craniotomy approaches carry higher morbidity and require longer hospital stays," says Dr. Wagner. "The transorbital route and collaboration between orbital surgeons and neurosurgeons allow access to otherwise difficult-to-reach lesions in the orbital apex and skull base with decreased risk for surgical morbidity, better visualization and faster recovery."
"Working together to manage these cases is ultimately in the best interest of the patient," says Jamie J. Van Gompel, M.D., a neurosurgeon at Mayo Clinic in Rochester, Minnesota. "The transorbital route allows us to successfully excise the tumor with minimal complications while preserving eye function. Additionally, this approach has tremendous cosmetic advantages that positively impact a patient's overall well-being and recovery."
"Our multidisciplinary collaboration provides integrated evaluation, testing, imaging and consultation within a few days in order to determine if a patient is a candidate for this minimally invasive approach," says Dr. Wagner. "Working closely together across specialties allows patients to receive individualized care plans — taking their personal treatment goals and disease characteristics into consideration."
For more information
Refer a patient to Mayo Clinic.