Sept. 26, 2024
Treatment of a CSF leak sometimes causes rebound intracranial hypertension, which is usually transient. But Mayo Clinic specialists have seen patients whose rebound hypertension is severe and recalcitrant. That scenario might indicate a primary condition of idiopathic intracranial hypertension, called IIH, that requires its own treatment.
"We have begun to appreciate that patients with primary IIH can spring a skull base or spinal CSF leak as a form of self-treatment. After successful treatment of the leak, these patients can then go back into high pressure. They might spring another CSF leak if the primary underlying high pressure isn't addressed," says Jeremy K. Cutsforth-Gregory, M.D., a neurologist and director of the CSF dynamics clinic at Mayo Clinic in Rochester, Minnesota.
Managing the complex overlap of IIH and CSF leaks requires a comprehensive, multidisciplinary approach. The CSF dynamics clinic brings together specialists with expertise in conditions involving both intracranial hypertension and hypotension.
"We are unique in that we have engagement across Neurology, Neurosurgery, ENT surgery, Ophthalmology and Radiology," Dr. Cutsforth-Gergory says. "Our neurologists are like orchestra conductors, calling on the advanced technologies and treatments available from each section to meet the patient's particular needs."
Benefits of a wide-angle view
Patients with spinal CSF leaks typically present with headaches that originate in the back of the head and worsen during the day. "After successful treatment, some patients have high-pressure symptomology for a few days or a week. The pendulum is swinging from too little CSF in the head to too much, before the pressure problems reequilibrate," Dr. Cutsforth-Gregory says.
But specialists in the CSF dynamics clinic began seeing patients whose post-treatment intracranial hypertension never resolved and sometimes even worsened. "These individuals might be stuck on pressure-lowering medications for weeks or months and might have refractory papilledema," Dr. Cutsforth-Gregory says.
The patients' headaches differed from those that led to their CSF leak diagnoses. Instead of back-of-the-head pain that worsened during the day, these individuals had pain at the front of the head that was worse overnight and on waking.
"Patients told us, 'Now my headaches are coming on while I'm lying down. That used to be when they'd get better,' " Dr. Cutsforth-Gregory says. "These individuals presented similarly to patients whose primary condition is IIH. After seeing that a few times, we realized we had missed an initial presentation of high-pressure disease. We were seeing these patients when they were experiencing symptoms of CSF leaks that had occurred as a result of IIH."
"Our neurologists are like orchestra conductors, calling on the advanced technologies and treatments available from each section to meet the patient's particular needs."
Precise diagnosis of underlying disease is a cornerstone of Mayo Clinic's approach. It requires a multidisciplinary team of experts who together can consider every aspect of a patient's condition. The CSF dynamics clinic exemplifies this patient-centered approach. It was founded by the late Bahram Mokri, M.D., a Mayo Clinic neurologist and pioneer in the field of CSF leaks. The care team includes neurologists, neuroradiologists, neurosurgeons and neuro-ophthalmologists who manage patients with the range of CSF pressure problems.
"Dr. Mokri thought we would learn something if we saw high-pressure and low-pressure patients in the same setting," Dr. Cutsforth-Gregory says. "That's exactly what has happened."
Innovative imaging and treatment
Specialists in the CSF dynamics clinic use the latest technology to localize CSF-venous fistulas, called CVFs. Although they are a common cause of CSF leaks, CVFs are notoriously difficult to localize. "CVFs are treatable — when we can find them," says Ajay A. Madhavan, M.D., a neuroradiologist at Mayo Clinic's campus in Minnesota.
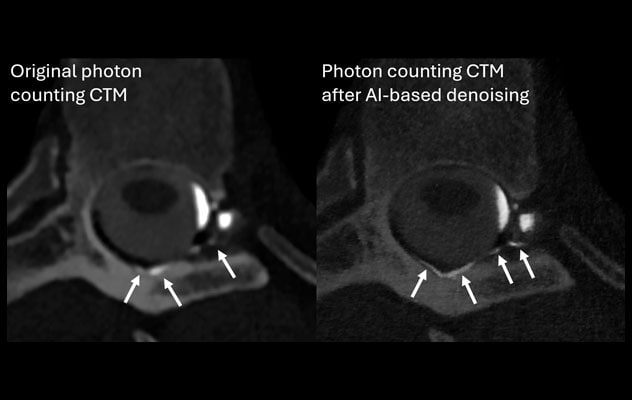
In 2023, Mayo Clinic began performing photon-counting detector CT myelography, called CTM, to identify CVFs. Photon-counting CTM's enhanced spatial resolution, fast scanning times and multienergy imaging allow neuroradiologists to identify abnormalities that can go undetected even on digital subtraction myelography. That technology is considered state-of-the-art at other specialty centers. In a review article in the American Journal of Neuroradiology, Mayo Clinic neuroradiologists discuss optimal CSF leak imaging modalities, including photon-counting CTM.
"Photon-counting CTM has provided us with a lot of benefit," Dr. Madhavan says. "We've performed well over 200 photon-counting CT myelograms in the last 18 months. It is quite common for us to find a CVF that was not visible on other techniques we commonly use. In particular, CVFs involving the internal epidural venous plexus are much easier to see on photon-counting CTM."
 التصوير المقطعي المحوسب للنخاع المحسَّن بالذكاء الاصطناعي
التصوير المقطعي المحوسب للنخاع المحسَّن بالذكاء الاصطناعي
صورتان ملتقطتان بتقنية التصوير المقطعي المحوسب بحساب عدد الفوتونات لنخاع مريض مصاب بناسور وريدي في الجانب الأيسر من السائل الدماغي النخاعي ينزح في الضفيرة الوريدية فوق الجافية الداخلية الظهرية. الصورة اليسرى: يصعب تمييز الناسور الوريدي في السائل الدماغي النخاعي في صورة النخاع المقطعية المحوسبة العادية بسبب التقارب بين الوريد النازح والعظمة الفقرية المجاورة له (موضح بالأسهم). والصورة اليمنى: بعد توضيح الصورة وتطبيق خوارزمية جديدة قائمة على التعلم العميق لإزالة الضوضاء من الصورة، زاد وضوح الناسور بشكل ملحوظ (موضح بالأسهم).
A novel deep learning-based algorithm has further improved image quality. As described in the American Journal of Neuroradiology, Mayo Clinic's application of the algorithm denoises photon-counting CTM images to maximize their spatial resolution. The enhanced technique was used to identify a CVF in a patient who experienced rebound intracranial hypertension after treatment of a CVF several years earlier. The rebound intracranial hypertension caused her to develop a new CVF, which again resulted in intracranial hypotension.
Mayo Clinic also has developed a minimally invasive procedure for treating CVFs. Transvenous embolization stops CSF leakage into blood vessels by gluing shut the fistula from inside the affected vein. "That allows us to avoid surgery in most cases," Dr. Cutsforth-Gregory says.
The goal is to provide each patient with precise diagnosis and a comprehensive, individualized treatment plan. "Working together, we can often solve these problems," Dr. Cutsforth-Gregory says. "That's not to say it's always an easy or one-time fix. But we strive to address all of our patients' needs as they arise."
For more information
Madhavan AA, et al. Myelographic techniques for the localization of CSF-venous fistulas: Updates in 2024. American Journal of Neuroradiology. In press.
Madhavan AA, et al. Application of a denoising high-resolution deep convolutional neural network to improve conspicuity of CSF-venous fistulas on photon-counting CT myelography. American Journal of Neuroradiology. 2023;45:96.
Refer a patient to Mayo Clinic.