Oct. 26, 2021
Mayo Clinic is one of only a few centers in the United States to have performed Gamma Knife radiosurgery on more than 10,000 patients. That extensive experience facilitates treatment for individuals with even the most challenging benign and malignant tumors.
الأورام شديدة الصعوبة
الأورام شديدة الصعوبة
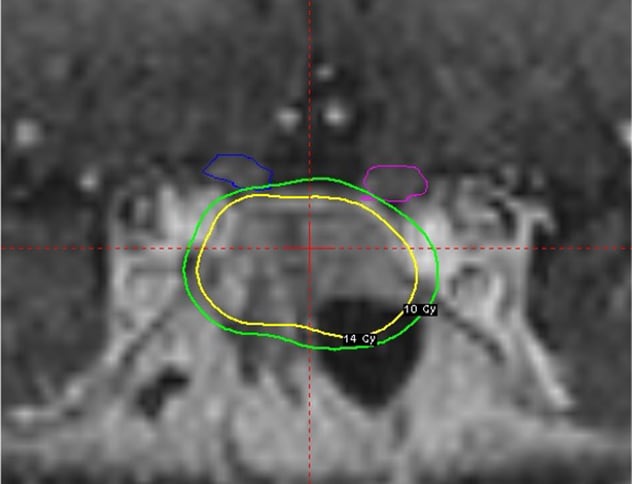
خطة جرعات جراحة إشعاعية لسيدة تبلغ من العمر 60 عامًا مصابة بأورام غدّية نخامية غير وظيفية، تظهر ملامسة الورم للعصب البصري الأيمن وعلى مسافة اثنين ملليمتر من العصب البصري الأيسر. وقد عُولج الورم بجرعة حدها الأدنى 14 غراي. وبلغ الحد الأقصى للجرعة الموجهة للعصب البصري 12.1 جراي.
"We routinely treat people who would typically be deferred from having Gamma Knife radiosurgery due to the size or location of their tumors," says Bruce E. Pollock, M.D., a neurosurgeon in the Brain Tumor Program at Mayo Clinic in Rochester, Minnesota. "For example, we often treat tumors contacting with the optic nerve that other centers would manage with either fractionated radiation therapy or surgical removal."
Although metastatic brain disease is the most common indication for Gamma Knife radiosurgery, Mayo Clinic has broad experience with the procedure for the treatment of vascular malformations, vestibular schwannomas and functional disorders such as trigeminal neuralgia. Data from Mayo Clinic's Gamma Knife radiosurgeries cover more than three decades, allowing clinician-researchers to publish extensively on the procedure.
"We've had a prospective patient registry from the start of the Gamma Knife project, and we continue to gather data for all patients who are treated," Dr. Pollock says. "With proper selection, we've been able to achieve tumor control rates in over 90% of cases."
Setting the standards
Mayo Clinic installed its first Gamma Knife in 1990. Fifty-seven patients, constituting 2% of all neurosurgical procedures, had the procedure that year. Mayo Clinic now treats more than 500 patients a year with Gamma Knife radiosurgery — approximately 10% of all neurosurgical operations.
Patient selection is key. "We review all patients to be sure that Gamma Knife radiosurgery is the best approach," Dr. Pollock says. "The surgeons involved with our Gamma Knife procedures also perform microsurgery — we operate as well as do radiation — and we strive to choose the optimal approach for each individual."
When Gamma Knife radiosurgery is indicated, Mayo Clinic's fully integrated practice fosters a multidisciplinary approach. "We have a close working relationship with our radiation oncologists, radiation physicists and specialized nursing staff," Dr. Pollock says. "Our MRI group allows rapid access to imaging, so our Gamma Knife procedures flow pretty quickly. That helps to get patients through the day in a nonstressful fashion."
As an early adopter of Gamma Knife radiosurgery, Mayo Clinic has been at the forefront of developing standards for the technology's use. In a landmark study, Mayo Clinic researchers found that patients with up to three brain metastases who had only stereotactic radiosurgery experienced less cognitive decline than patients who had stereotactic radiosurgery combined with whole-brain radiation therapy. That study was published in the July 26, 2016, issue of JAMA. More recently, in a study to be published in Neuro-Oncology Advances, Mayo Clinic researchers found that stereotactic radiosurgery is an effective salvage treatment in nodular leptomeningeal recurrence.
Among several projects involving arteriovenous malformations, the results of a study published in the May 2021 issue of Mayo Clinic Proceedings demonstrated that biological effective dose is associated with the likelihood of obliteration of cerebral arteriovenous malformations following single-session Gamma Knife radiosurgery.
"The growth and utilization of radiosurgery is likely to continue as more data become available on the long-term results of this procedure," Dr. Pollock says. "Significant advances in neuroimaging, dose planning software and radiation delivery approaches have improved patient outcomes for a wide variety of benign and malignant tumors, vascular malformations, and functional disorders."
For more information
Brown PD, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: A randomized clinical trial. JAMA. 2016;316:401.
Teyateeti A, et al. Outcome comparison of patients who develop leptomeningeal disease or distant brain recurrence after brain metastases resection cavity radiosurgery. Neuro-Oncology Advances. In press.
Nesvick CL, et al. The role of biological effective dose in predicting obliteration after stereotactic radiosurgery of cerebral arteriovenous malformations. Mayo Clinic Proceedings. 2021;96:1157.