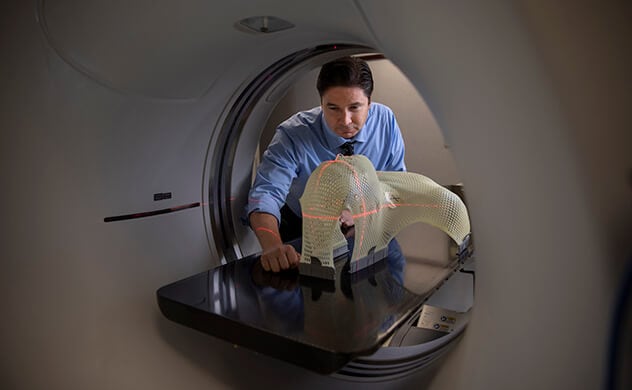
Radiation oncology medical physicist Chris J. Beltran, Ph.D., works with a 3D model to develop better options for people who need radiation treatment.
If you are prescribed radiation therapy to treat your cancer, a radiation oncology medical physicist is a key member of your care team. The radiation oncology medical physicist works with members of your radiation oncology team, including:
With your care team, radiation oncology medical physicists apply their knowledge of radiation physics to radiation biology. They ensure you receive the exact dose of radiation you need, targeted and delivered exactly where you need it.
Customizing your care
Radiation oncology medical physicists are involved at the earliest stages of your cancer care. After your team understands your specific type of cancer, they use a computerized tomography scan, also called a CT scan, to create a 3D radiation treatment plan specific to you and your cancer. During the CT scanning process, your team creates immobilizing devices custom-made to your body type and the treatment you receive.
Radiation oncology medical physicists check that the type of immobilizing devices are specific to your needs and that the devices are working properly. They also check that the devices are set up properly, so the radiation machine delivers accurate, consistent doses every time you receive treatment.
Radiation oncology medical physicists collaborate with your radiation oncology team to make sure radiation treatments are planned to deliver the most-effective dose to the tumor while sparing as much healthy tissue surrounding the tumor as possible. They work with radiation therapists to make sure the doses are delivered as precisely as possible.
Types of radiation therapy
At Mayo Clinic, many forms of radiation therapy are available. Your team will tailor treatment options to your cancer and your needs. The treatments that radiation oncology medical physicists help deliver include:
- External beam therapy using photons, which is the most common form of radiation therapy.
- External beam therapy using particles, including proton beam therapy.
- Brachytherapy, also called internal radiation therapy.
- Intraoperative radiation therapy, which is external or internal radiation treatment during surgical removal of a tumor.
- Nuclear medicine therapy, which is radiation delivered through IV or a capsule.
If you require brachytherapy, which involves placing radioactive material inside the body through needles or a device placed within your body, a radiation oncology medical physicist collaborates with your care team. Together, they tailor the treatment based on many factors, such as:
- Tumor characteristics.
- The optimal radiation dose.
- Your body type.
The treatment, sometimes called internal radiation therapy, allows your healthcare team to use higher doses of radiation than would be possible with external radiation. This is because brachytherapy delivers radiation directly to the treatment area, which lowers the risk of hurting healthy tissue that is nearby.
Enhancing your care
In addition to caring for patients, radiation oncology medical physicists ensure radiation delivery machines are calibrated correctly and working properly. They are responsible for maintaining daily, monthly and yearly quality assurance checks that adhere to state and federal Nuclear Regulatory Commission regulations. They also ensure Mayo Clinic uses the very latest and most effective radiation oncology practices.
When new technology or equipment become available, radiation oncology medical physicists make sure it is used safely and effectively. They develop standard operating procedures and train all Mayo Clinic staff who use the equipment.

Radiation oncology medical physicist, Deanna H. Pafundi, Ph.D., positions a radiation detector in a water tank to submillimeter accuracy to measure the radiation beam during yearly quality assurance checks.
Research
Radiation oncology medical physicists are heavily involved in cancer care research. Areas include:
- Radiobiological modeling, which helps predict how certain types of cancer cells will respond to different kinds of radiation. The goal is to make radiation therapies more effective while reducing side effects.
- Adapting new technology to make it safe and effective for patients.
- Computer modeling that uses artificial intelligence. Goals include making the treatment process more efficient and better predicting how each patient will respond to different types of radiation.
Education
Radiation oncology medical physicists also are involved with teaching the fundamental aspects of radiation physics, radiation safety principles and clinical applications of radiation therapy to residents, trainees and staff.
Doctors
Mayo Clinic has one of the largest and most experienced practices in the United States, with campuses in Arizona, Florida and Minnesota. Staff skilled in dozens of specialties work together to ensure quality care and successful recovery.