概述
活体肾移植术

活体肾移植术
在活体肾移植中,医生会摘除捐献者的一个健康肾脏,然后将其移植给肾脏不能正常运转的接受者。除非接受者自身肾脏导致并发症,否则将予以保留。
In a living-donor kidney transplant, a kidney is taken from a living person and given to someone who needs a kidney. The person who receives the kidney has kidneys that have failed and no longer work properly.
Only one kidney is needed for health. For this reason, a living person can donate a kidney and still live a healthy life. Living-donor kidney transplant is an alternative to receiving a kidney from someone who has died. A relative, friend or even a stranger may donate a kidney to someone in need.
About one-third of all kidney transplants performed each year in the U.S. are living-donor kidney transplants. The other two-thirds involve a kidney from a deceased donor.
Many people need a kidney. More than 139,000 people were on the national waiting list for a kidney in 2021.
Types
目的
People with end-stage kidney disease have kidneys that no longer work. People with end-stage kidney disease need to have waste removed from their bloodstream to stay alive. Waste can be removed through a machine in a process called dialysis. Or a person can receive a kidney transplant.
For most people with advanced kidney disease or kidney failure, a kidney transplant is the preferred treatment. Compared to a lifetime on dialysis, a kidney transplant offers a lower risk of death and more dietary options than dialysis.
There are some benefits to having a living-donor kidney transplant instead of a deceased-donor kidney transplant. The benefits of a living-donor kidney transplant include:
- A shorter waiting time. Less time on the national waiting list may prevent a decline in the health of the person who needs a kidney.
- Avoiding dialysis if it has not been started.
- Better survival rates.
- The transplant may be scheduled ahead of time once the donor is approved. Transplant surgery is unscheduled and urgent when a deceased-donor kidney becomes available.
风险
开始您的供体评估
要成为活体肾脏捐献者或活体肝脏捐献者,首先请完成这份健康史问卷。
The risks of living-donor kidney transplant are like the risks of deceased-donor kidney transplant. Some are similar to the risks of any surgery. Others have to do with organ rejection and side effects of drugs that prevent rejection. Risks include:
- Pain.
- Infection at incision site.
- Bleeding.
- Blood clots.
- Organ rejection. This is marked by fever, feeling tired, low urine output, and pain and tenderness around the new kidney.
- Side effects of anti-rejection drugs. These include hair growth, acne, weight gain, cancer and increased risk of infections.
如何进行准备
If your doctor recommends a kidney transplant, you'll be referred to a transplant center. You can choose a transplant center on your own or choose a center from your insurance company's list of preferred providers.
After you choose a transplant center, you'll be evaluated to see if you meet the center's eligibility criteria. The evaluation may take several days and includes:
- A complete physical exam.
- Imaging tests, such as X-ray, MRI or CT scans.
- Blood tests.
- Cancer screening.
- Psychological evaluation.
- Evaluation of social and financial support.
- Any other tests based on your health history.
可能出现的情况
配对器官捐献
配对器官捐献
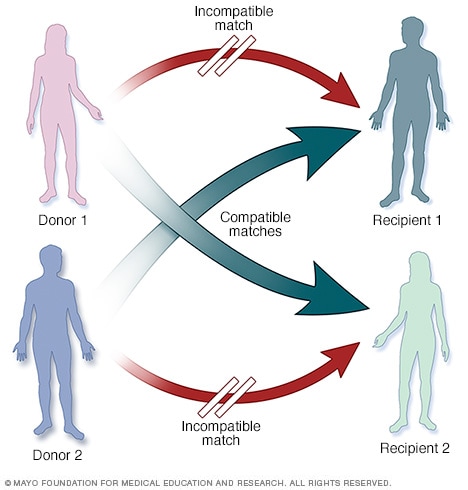
在配对器官捐献中,活体供体及其受体不相容,不能进行移植。但每对中的供体分别与另一对中的受体相容。如果供体和受体都愿意,医生可能会考虑配对器官捐献。
Living-donor kidney transplant usually involves a donated kidney from someone you know. It might be a family member, friend or co-worker. Family members related by blood are usually the most compatible living kidney donors.
A living kidney donor also may be someone you don't know. This is called a non-directed living kidney donor.
A living donor who wants to give you a kidney will be evaluated at the transplant center. If the person is cleared for donation, tests will be done to see if that person's kidney is a good match for you. In general, your blood and tissue type need to be compatible with the donor. If the donor kidney is a good match, your transplant surgery will be scheduled.
If the donor's kidney is not a good match, there are several options. In some cases, your transplant team can use medical treatments to help your immune system adjust to the new kidney before and after the transplant to reduce the risk of rejection.
Another option is taking part in a paired donation. Your donor may give a kidney to another person who is a good match. Then you receive a compatible kidney from that recipient's donor. This type of exchange often involves more than two pairs of donors and recipients, resulting in several people receiving a kidney.
Once you and your donor are cleared for surgery, the transplant team will schedule your transplant surgery. They also will make sure you are still in overall good health and confirm that the kidney is a match for you. If everything looks good, you'll be prepped for surgery.
During surgery, the donor kidney is placed in your lower abdomen. Blood vessels of the new kidney are attached to blood vessels in the lower part of your abdomen, just above one of your legs. The surgeon also connects the tube from the new kidney to your bladder to allow urine flow. This tube is called the ureter. The surgeon usually leaves your own kidneys in place.
You'll spend several days to a week in the hospital. Your healthcare team will explain what medicines you need to take. They also will tell you what problems to look out for.
Once you've been matched with a living kidney donor, the kidney transplant procedure will be scheduled in advance. The kidney donation surgery (donor nephrectomy) and your transplant typically occur on the same day.
结果
After a successful kidney transplant, your new kidney will filter your blood and remove waste. You will not need dialysis.
You will take medicines to prevent your body from rejecting your donor kidney. These anti-rejection medicines suppress your immune system. That makes your body more likely to get an infection. As a result, your doctor may prescribe antibacterial, antiviral and antifungal medicines.
It is important to take all your medicines as your doctor prescribes. Your body may reject your new kidney if you skip your medicines even for a short period of time. Contact your transplant team immediately if you have side effects that keep you from taking the medicines.
After the transplant, be sure to perform skin self-checks and get checkups with a dermatologist to screen for skin cancer. Also, staying up to date with other cancer screenings is strongly advised.
临床试验
探索 Mayo Clinic 的研究 测试新的治疗、干预与检查方法,旨在预防、检测、治疗或控制这种疾病。