July 25, 2024
Approximately 10% of renal cell carcinomas (RCCs) will have a venous tumor thrombus (VTT) growing into the renal vein or inferior vena cava (IVC). The surgical treatment of RCC with VTT is challenging and has a high risk of cancer recurrence. Thus, improving surgical and oncologic outcomes for patients with RCC and VTT is a critical unmet need in urologic oncology. Vidit Sharma, M.D., a urologist at Mayo Clinic in Rochester, Minnesota, specializes in the surgical treatment of advanced renal tumors, including those with VTT. Dr. Sharma's work was recently selected for the American Urological Association (AUA) 2024 Early-Career Investigators Showcase, and he received a two-year Urology Care Foundation grant to improve outcomes for patients with venous tumor thrombus.
Dr. Sharma's findings are summarized below:
National estimate of in-hospital complications after nephrectomy with VTT versus hospital volume
VTT 患者的外科护理
VTT 患者的外科护理
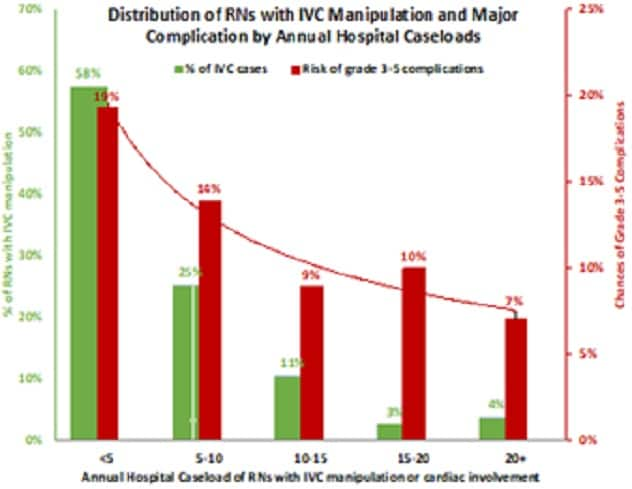
本图显示了按年度医院病例量统计的参与 IVC 操作和重大并发症诊治的注册护士分布情况。
This study identified 111,785 radical nephrectomies using the National (Nationwide) Inpatient Sample, of which 3.3% (N = 3691) had significant IVC manipulation and 0.3% (N = 335) had cardiac involvement. On multivariable regression, IVC manipulation (OR 1.56, p < 0.01) and cardiac involvement (OR 4.31, p < 0.01) were associated with major complications. Approximately 82% of VTT cases were performed at centers that perform fewer than 10 such cases per year. The risk of major complications was significantly lower if annual hospital VTT volume exceeded 10 on both chi-squared analysis (8.7% versus 17.6%, p < 0.01) and multivariable regression (OR 0.62, p = 0.04). Thus, centralization of surgical care for patients with VTT may improve complications.
VTT and surgical complications over time
To determine if surgical complications are improving for patients over time, researchers queried their registry for all adult patients who underwent radical nephrectomy for RCC with thrombectomy between 2000 and 2021 (N = 786). The risk of any complications for levels 0, 1, 2, 3 and 4 VTT was 11.9% (n = 49), 25.9% (n = 29), 29.1% (n = 46), 28% (n = 14) and 57.4% (n = 31), respectively, and perioperative death occurred in 0%, 0%, 1.3%, 6% and 7.4%, respectively. Dr. Sharma is investigating the use of 3D-printed, full-scale models of RCC with VTT in reducing the morbidity of surgery.
VTT demonstrates a metastatic tropism to the lungs in the presence of pulmonary embolus
肺转移
肺转移
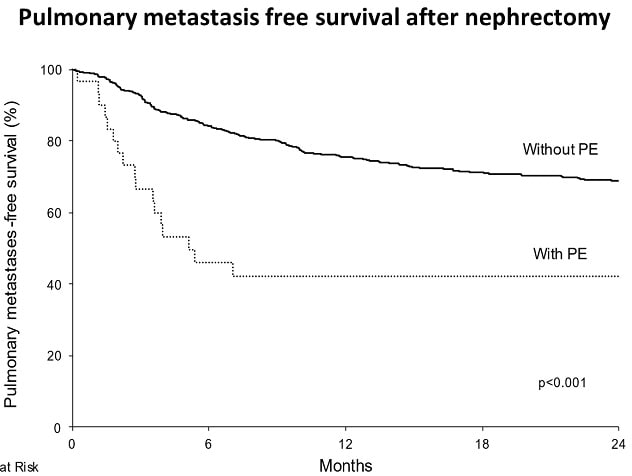
记录了有肺栓塞和无肺栓塞患者肾切除术后的无肺转移生存期。
Researchers queried their institutional registry for patients with clear cell RCC undergoing radical nephrectomy (1970 to 2019, n = 3,410) to determine whether VTT (N = 1,025) was associated with pulmonary metastases. VTT was associated with increased synchronous pulmonary metastases (20% versus 7%, p < 0.001). Excluding patients with pulmonary metastases at nephrectomy, VTT remained associated with an increased risk of developing metachronous pulmonary metastases (multivariable HR 1.31, p < 0.001). For patients with VTT, pre-op pulmonary embolus was associated with an increased risk of pulmonary metastases postnephrectomy (HR 2.31, p < 0.001). These results support a metastatic predilection of clear cell RCC with VTT to the lungs and argue for judicious VTT manipulation intraoperatively to minimize risk of pulmonary embolus.
Evaluating VTT as a criterion for adjuvant pembrolizumab use after radical nephrectomy
无转移生存期
无转移生存期
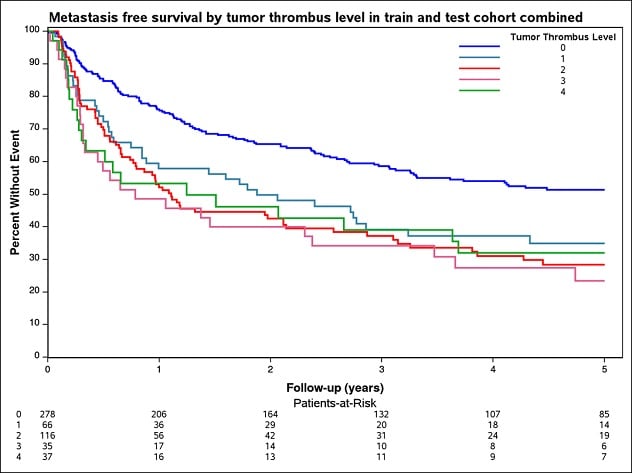
本图显示了训练和测试合并队列中按癌栓水平划分的无转移生存期。
Adjuvant pembrolizumab was recently confirmed to have an overall survival benefit for advanced clear cell RCC. Dr. Sharma recently published a simulation model balancing the risks and benefits of adjuvant pembrolizumab to determine that its benefits outweighed the harms for patients with a five-year risk of metastasis of at least 60%. In this abstract, Dr. Sharma examined the institutional VTT experience (N = 786) to create a nomogram for metastasis-free survival after nephrectomy for VTT to identify why adjuvant therapy would be recommended.
The five-year risk of metastasis for level 0 and levels 1 to 4 VTT was 50% and 60% to 80%, respectively. Researchers created and internally validated a nomogram to identify features associated with metastasis after surgery. Using this nomogram, patients with levels 0 to 2 VTT without necrosis, sarcomatoid features or positive nodes did not meet the 60% five-year metastasis threshold to warrant adjuvant pembrolizumab.
VTT has a high risk of complications nationally. However, high-volume centers were found to have a lower risk of complications and referral of these patients to high-volume centers may improve outcomes. Dr. Sharma is investigating the use of 3D-printed models in reducing the morbidity of surgery. Oncologic outcomes can be improved by using adjuvant pembrolizumab for certain subsets of patients with VTT. Given the predilection of VTT to metastasize to the lung, particularly in the context of pulmonary embolism, minimizing thrombus manipulation before IVC clamping is prudent from an oncologic perspective. Together these findings set the stage for future studies to improve outcomes for RCC with VTT.
For more information
Refer a patient to Mayo Clinic.