Jan. 31, 2020
Specialists at Mayo Clinic Children's Center in Rochester, Minnesota, are seeking innovations for children with epilepsy, while research teams are studying potential treatments, including new medications and surgical options. As a result, several cutting-edge options to eliminate or reduce seizures in children are available.
"Experts from various specialties are coming together to make decisions about medications and treatments," says Kai J. Miller, M.D., Ph.D., a neurosurgeon at Mayo Clinic Children's Center. "The research and clinical teams function seamlessly together. As a result, patients receive the most novel therapies to treat seizures and preserve brain function. Together, we're actively developing new technology."
Evaluation and treatment
Mayo Clinic Children's Center has a pediatric team dedicated to the care of children with epilepsy. After an initial evaluation, children and their parents can choose from a number of available options to reduce seizure frequency and severity.
"For some children with drug-resistant epilepsy, surgery is an option. But for others, a unique type of medication or diet therapy can decrease seizure frequency and severity," says Elaine C. Wirrell, M.D., a pediatric epileptologist at Mayo Clinic Children's Center and co-founder of the Pediatric Epilepsy Research Consortium.
Epilepsy surgery: Treatment when medicine doesn't work
Epilepsy surgery, which is considered when at least two anti-seizure medications have failed to work, removes or alters an area of the brain where seizures originate. As a Level 4 Comprehensive Epilepsy Center, the highest rating designated by the National Association of Epilepsy Centers, Mayo Clinic's multidisciplinary team works to improve outcomes and reduce hospital stays through minimally invasive and advanced surgical techniques, including robotic guidance surgery.
"Using robotic guidance, surgeons can more precisely identify where seizures start," says Dr. Miller. "This allows us to target the seizures and stop them."
Resective surgery
With resective epilepsy surgery, surgeons remove a focal area of abnormal brain tissue that generates seizures. Surgery is most often performed on either the frontal lobe, an area controlling motor and language function, or the temporal lobe, an area that controls memory, comprehension and emotions. In some children, resective surgery requires a larger operation. However, a much less invasive technique called laser interstitial thermal therapy may be an option for some children. In this technique, MRI is used to guide the surgeon to place a probe through a small hole in the skull. A laser pinpoints and destroys a small portion of brain tissue.
"This therapy actually burns and destroys the place in the brain where the seizure originates," explains Dr. Miller. "And it does so without injuring the rest of the brain or requiring a large surgery."
Corpus callosotomy
Used in children who experience frequent drop seizures leading to repeated and abrupt falls, this surgery severs the bundle of nerves connecting the right and left sides of the brain. In most cases, the drop seizures are eliminated or markedly decreased, preventing ongoing injury.
Hemispherectomy
Children who experience seizures that originate from multiple sites in one hemisphere often require a functional hemispherotomy. This surgery disconnects the abnormal, seizure-inducing hemisphere, allowing the other hemisphere to function normally and stopping the seizures.
Neurostimulation treatments
Experts at Mayo Clinic Children's Center are also studying neurostimulation treatments for epilepsy, an alternative treatment for children with severe epilepsy or for those who cannot have surgery. This treatment applies electricity to the central nervous system with the goal of reducing seizure frequency and severity.
Some neurostimulation treatments are invasive, meaning they require a surgical procedure to implant a device. With these treatments, an internal pulse generator or neurostimulator supplies electricity via an extension to implanted electrodes.
Vagus nerve stimulation
Vagus nerve stimulation prevents seizures by sending regular, mild pulses of electrical energy to the brain via the vagus nerve. A stimulator device is implanted under the skin in the chest, and a wire is wound around the vagus nerve in the neck.
Responsive neurostimulation
Responsive neurostimulation works by monitoring brain waves and responding to electrical activity that looks like a seizure to stop seizures before they cause clinical symptoms.
Deep brain stimulation
Mayo Clinic is one of the leading sites in the country for deep brain stimulation implantation. This therapy delivers controlled pulses to a target in the brain that is part of a circuit involved in seizures.
长期阈下皮质刺激

长期阈下皮质刺激
慢性阈下皮质刺激利用通过外科手术植入于癫痫发作部位的电极。这些电极会与已植入胸部的发生器连接。
Chronic subthreshold cortical stimulation
In some cases, by the time a responsive device detects abnormal electrical activity, it might be too late to prevent a seizure. Subthreshold cortical stimulation provides continuous electrical impulses to an area of seizure onset to suppress the generation of the abnormal seizure discharge and thus attenuate the seizure.
An article co-authored by Dr. Miller and published in the October 2019 issue of Brain Sciences reported that chronic subthreshold cortical stimulation resulted in a progressive decline in the frequency of seizures in a group of 10 patients. "The frequency of seizures and interictal discharges showed a progressive decline during continuous stimulation," the article states. Furthermore, the article highlights "a greater than 90% seizure reduction in two patients with a simulation of the eloquent motor cortex for about one year."
重复性经颅磁刺激
重复性经颅磁刺激
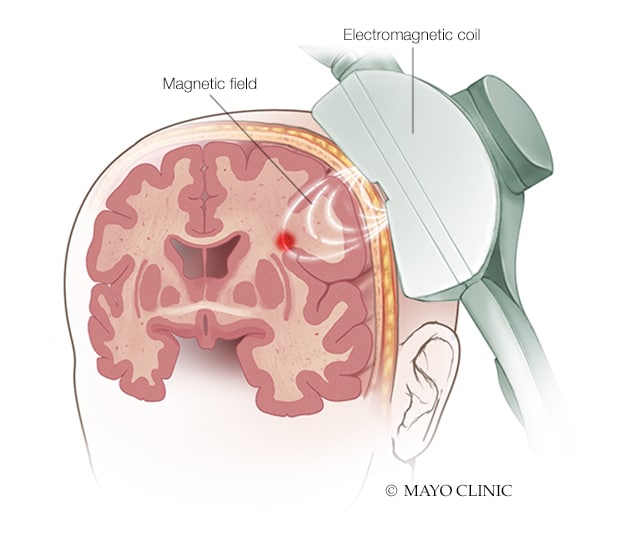
在经颅磁刺激中,置于头皮上的电磁线圈产生磁场,刺激大脑的某些区域。
Transcranial magnetic stimulation
During a transcranial magnetic stimulation session, an electromagnetic coil placed against the scalp delivers a magnetic pulse that stimulates nerve cells in the brain.
Transcranial direct current stimulation
Transcranial direct current stimulation applies a low-intensity current that manipulates neuronal activity and neuroplasticity.
Cutting-edge treatments and clinical trials
While surgical and neurostimulation treatments focus on seizure control, Mayo Clinic's multidisciplinary team of experts are researching cutting-edge drug treatments and participating in multiple clinical trials for the treatment of severe epilepsy syndromes. These include Dravet syndrome and Lennox-Gastaut syndrome, rare but severe epilepsy syndromes.
"As neurologists, we provide precision therapies through advanced understanding of etiologies and preferred treatments, such as potassium channel blockers for patients with potassium channel-related epilepsy encephalopathies and stiripentol and cannabidiol for patients with Dravet syndrome," explains Katherine C. Nickels, M.D., a pediatric epileptologist at Mayo Clinic Children's Center in Rochester, Minnesota. "While many of these therapies are considered to be new in most institutions, they are the standard of care here."
In an article in the September 2019 issue of CNS Drugs, Dr. Wirrell and colleagues discussed promising results with drugs for Dravet syndrome, including stiripentol. "Stiripentol was associated with a greater than 50% reduction in convulsive seizure frequency in 71% of patients," their study showed.
In addition to focusing on medical treatments, the Mayo team provides holistic care for the child and family, addressing the learning and behavioral challenges that often are seen.
For more information
Pediatric Epilepsy Research Consortium.
Starnes K, et al. A review of neurostimulation for epilepsy in pediatrics. Brain Sciences. 2019;9:283.
Wirrell EC, et al. Recent advances in the drug treatment of Dravet syndrome. CNS Drugs. 2019;33:867.