Aug. 30, 2024
Mayo Clinic Children's Center is committed to using cutting-edge, minimally invasive approaches to pediatric epilepsy. As a level 4 comprehensive epilepsy center, Mayo Clinic offers a range of treatment options that address all aspects of children's care.
"A quaternary facility with multiple specialists can provide treatment not just for seizures but also for comorbidities," says Lily C. Wong-Kisiel, M.D., a pediatric epileptologist at Mayo Clinic in Rochester, Minnesota. "Patients seeking initial treatment or second opinions benefit from that experience and expertise."
Level 4 is the highest rating designated by the National Association of Epilepsy Centers. In addition to providing extensive medical and surgical treatments, a level 4 center offers sophisticated neurodiagnostic monitoring and neuropsychological and psychosocial therapies. At Mayo Clinic, neurodiagnostic monitoring includes minimally invasive stereo electroencephalography (sEEG). Minimally invasive treatment might involve laser interstitial thermal therapy (LITT) or neurostimulation.
Mayo Clinic epileptologists are active in national groups associated with clinical trials for rare genetic epilepsies such as Dravet syndrome. "Children with this condition survive into adulthood, and we have adult epileptologists who are familiar with Dravet syndrome," Dr. Wong-Kisiel says. "It's important to transition these patients to lifelong care."
Thorough diagnostic imaging
Mayo Clinic has extensive experience with the use of sEEG to localize seizure onset sites in children. "High-quality brain imaging is critical prior to sEEG to guide electrode implantation," says Mayo Clinic neuroradiologist Brian J. Burkett, M.D., M.P.H.
 优化的癫痫成像方案
优化的癫痫成像方案
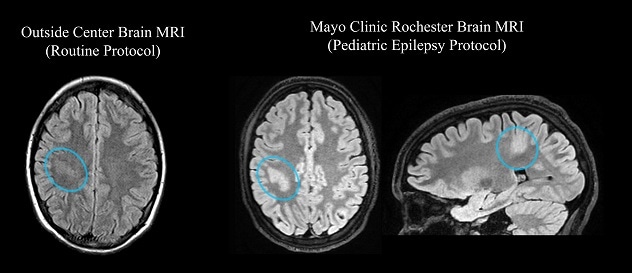
一名 14 岁癫痫患者的 MRI 图像。左图。一张来自其他机构的图像,图中病变(蓝色圆圈标注)难以辨认。右图。使用妙佑医疗国际的优化 MRI 方案做 MRI,病变(蓝色圆圈标注)清晰可见。专用癫痫成像方案包括三维图像采集,从而能够在多个空间平面中确认病变。
Mayo Clinic specialists use an MRI protocol specific to pediatric epilepsy. The protocol is optimized to show various types of abnormalities that might cause seizures.
"In many cases, these abnormalities are subtle and could be obscured or even invisible on an MRI of lower quality," Dr. Burkett says. "Review by experienced neuroradiologists also maximizes the chance of detecting abnormalities. Prior to sEEG, cases are reviewed by several Mayo Clinic neuroradiologists with expertise in epilepsy imaging."
Additional brain imaging techniques that might be used include:
- Skull base CT.
- Subtracted ictal and inter-ictal SPECT (SISCOM) and statistically normalized subtraction coregistered to MRI (STATISCOM).
- Positron emission tomography (PET)-CT.
- PET-MRI.
"Mayo Clinic can provide options that might not be available elsewhere."
Localizing seizure onset sites with sEEG means children avoid craniotomy and generally have shorter hospital stays. "Once the electrodes are removed, patients often leave the hospital the next day," Dr. Wong-Kisiel says.
sEEG also allows more time to consider treatment options. "Since there's no craniotomy, the decision about therapy doesn't need to be made right away," Dr. Wong-Kisiel says. "Surgery is a big step. sEEG allows parents more time to be comfortable with making decisions."
The procedure might be combined with ablation. "There is an option to add radiofrequency ablation to the electrodes that are recording during sEEG in areas identified as seizure focus sites," Dr. Wong-Kisiel says. "About 40% of patients might have some benefit in terms of seizure reduction."
Minimally invasive treatments
Once neurodiagnostic monitoring is completed, Mayo Clinic's pediatric epilepsy team meets to determine optimal treatment. LITT may be used to ablate focal epileptogenic regions previously treated with an open craniotomy approach.
Corpus callosotomy might be considered for children experiencing generalized onset atonic or tonic seizures. The procedure eliminates or markedly decreases these drop seizures for most children. Mayo Clinic subspecialists have experience using LITT to perform corpus callosotomy. "Laser callosotomy is significantly less invasive than open callosotomy, which involves craniotomy, dissection and brain retraction," says Mayo Clinic pediatric neurosurgeon Kai J. Miller, M.D., Ph.D.
Neurostimulation therapies, which aren't commonly used to treat pediatric epilepsy, also are an option for focal and generalized epilepsy. Stimulation might be trialed in areas indicated by sEEG during that procedure. Mayo Clinic offers responsive neurostimulation, deep brain stimulation, vagus nerve stimulation and subthreshold cortical stimulation.
"Our goal is to get rare disease patients to therapeutic opportunities."
Mayo Clinic also uses two types of noninvasive neurostimulation: transcranial magnetic stimulation for children with highly focal seizure origin sites; and direct current stimulation for children with multiple seizure origin sites or a single, broad seizure origin site.
"Noninvasive stimulation is potentially a very appealing option for children with drug-resistant epilepsy whose families are hesitant regarding a more invasive and permanent device implant," says Mayo Clinic pediatric neurologist Keith K. Starnes II, M.D.
Rare developmental epilepsies
Mayo Clinic's epileptologists study innovative therapies to treat rare but severe epilepsy syndromes. Clinical trials might be available. "Mayo Clinic has participated in many of the placebo-controlled clinical trials for antiseizure medications," Dr. Wong-Kisiel says.
Mayo Clinic clinicians also work with researchers in the Center for Individualized Medicine to develop treatments for children with nano-rare seizure disorders. "Our goal is to get rare disease patients to therapeutic opportunities," says Margot A. Cousin, Ph.D., who directs the center's N-of-1 Therapeutics program.
A primary focus is developing custom antisense oligonucleotide (ASO) therapies directed against individuals' specific genetic mutations. ASOs are synthetic and chemically modified oligonucleotides that can alter RNA and modify protein function and expression. "Increasingly, we are realizing that we can develop these types of gene-targeted therapies for individual patients when currently available therapies fail or are insufficient," Dr. Cousin says.
The interaction between clinicians and researchers underlies Mayo Clinic's commitment to innovative care. "Mayo Clinic can provide options that might not be available elsewhere," Dr. Wong-Kisiel says.
For more information
Children's Center. Mayo Clinic
Center for Individualized Medicine. Mayo Clinic.
Refer a patient to Mayo Clinic.