Aug. 19, 2023
Endoscopic resection (ER) is a minimally invasive method of removing precancerous or early-stage, superficial esophageal lesions. Although endoscopic mucosal resection (EMR) is an effective first line therapy for removal of smaller lesions, lesions larger than 2 cm must be removed in pieces using this technique. Overcoming this limitation and others led to the development of a newer resection technique called endoscopic submucosal dissection (ESD).
In an article published in Gastroenterology Clinics of America in 2023, Mayo Clinic gastroenterologist Norio Fukami, M.D., describes indications, techniques and outcomes associated with esophageal ESD. Dr. Fukami is a therapeutic endoscopist at Mayo Clinic in Arizona. In this Q&A, Dr. Fukami answers a few key questions about ESD benefits and techniques.
What are some of the advantages of using ESD?
内镜黏膜下剥离术(ESD)
内镜黏膜下剥离术(ESD)
ESD 用于整体切除因过大而不适合内镜黏膜切除术的病变以及形状不规则的病变(包括多灶性或结节性病变),是一种非常有效的方法。ESD 需要使用专用刀片徒手操作,方便内镜医生控制切除组织的大小、形状和深度。
ESD is a highly effective method for performing en bloc removal of lesions that are too large for EMR and those with irregular shapes, including multifocal or nodular lesions. This approach involves using a dedicated knife (or knives) and a freehand technique, which allows endoscopists to control the size, shape and depth of the tissue resected.
By enabling the removal of a wider area of tissue, ESD can also facilitate improved pathological evaluation and better cancer risk stratification to guide further treatment and surveillance. When used as a cancer resection method, ESD offers more-precise margin determination and is an effective means of achieving negative margin resection for larger and more complex lesions to improve outcomes in patients with cancer.
How do the advantages associated with ESD advance the management of patients with esophageal squamous cell carcinoma or adenocarcinoma?
术前图像显示有食管腺癌

术前图像显示有食管腺癌
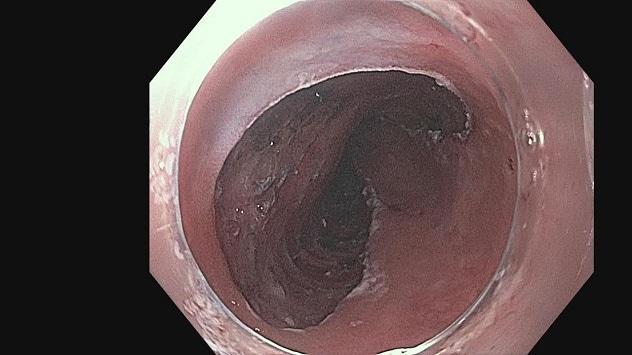
在一长段巴雷特食管内发现一个 3 cm 的结节。活检显示至少有黏膜内腺癌。
食管术后图像
食管术后图像
在内镜下黏膜下剥离术(ESD)过程中,整块切除了三分之二的结节,总共 5 cm。
Esophageal squamous cell carcinoma (ESCC) is often found when nodularity is apparent, and at this stage, cancer frequently involves muscularis mucosae or submucosa. Each level of invasion signifies a different level of risk of cancer spread. Endoscopic inspection may not differentiate between minute differences within mucosa. And it may not differentiate between mucosal disease and disease with shallow submucosal (SM) invasion. For risk stratification, ER provides precise pathological staging. ER also aims for curative resection, and thus, negative margin is required. Compared with EMR, ESD offers a more effective way to achieve negative margin resection for curative resection.
Adenocarcinoma arises within Barrett's esophagus or at the gastroesophageal junction and is often accompanied by a wider area of dysplasia. Similar to ESCC, precise staging of superficial cancer is best achieved with pathological evaluation to stratify risks of metastasis and the need for further therapy. Larger resection with ESD facilitates one-piece removal of cancer and dysplasia with negative margins more effectively than does EMR, offering sounder oncologic resection. ESD has been reported to improve subsequent Barrett's eradication therapy.
What is unique about performing ESD in the esophagus?
The esophagus is a tubular organ that can easily be accessed with an upper endoscope. Yet ESD in the esophagus demands a full understanding of anatomy, tools and techniques as well as well-trained skills. SM dissection can be rather effortless because it is aided by the natural angle of approach that is nearly parallel to the esophageal wall. Because the esophagus lacks a protective serosal layer, SM dissection should be performed well above muscularis propria to prevent muscle exposure or injury and reduce adverse events.
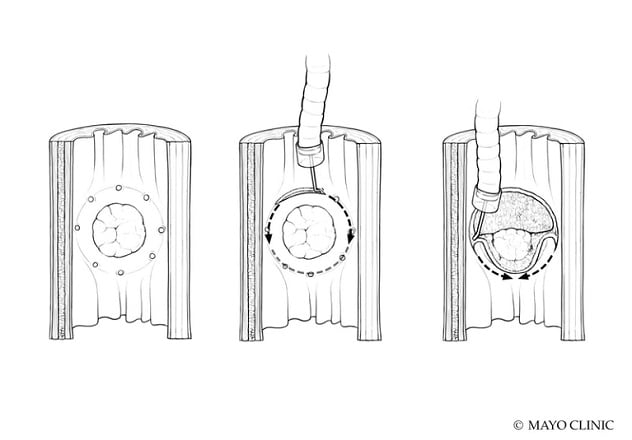
Can you describe the two main procedural approaches used during ESD?
The traditional method of ESD involves making a circumferential mucosal incision and completing the SM dissection afterward. An alternate approach, called the tunneling method, involves making the distal and proximal mucosal incisions, dissecting them down to the SM layer, and then completing the SM dissection from the proximal to distal end, creating a tunnel. We typically recommend dissection at the SM2 layer, the middle layer of the SM layer, unless SM invasion of cancer is suspected. General endotracheal anesthesia is used to sustain optimal airway control, respiratory effort and cardiac movement throughout the procedure.
For more information
Fukami, N. Endoscopic submucosal dissection in the esophagus: Indications, techniques, and outcomes. 2023;33:55.
Refer a patient to Mayo Clinic.