Aug. 19, 2023
Endoscopic resection (ER) is a minimally invasive method of removing precancerous or early-stage, superficial esophageal lesions. Although endoscopic mucosal resection (EMR) is an effective first line therapy for removal of smaller lesions, lesions larger than 2 cm must be removed in pieces using this technique. Overcoming this limitation and others led to the development of a newer resection technique called endoscopic submucosal dissection (ESD).
In an article published in Gastroenterology Clinics of America in 2023, Mayo Clinic gastroenterologist Norio Fukami, M.D., describes indications, techniques and outcomes associated with esophageal ESD. Dr. Fukami is a therapeutic endoscopist at Mayo Clinic in Arizona. In this Q&A, Dr. Fukami answers a few key questions about ESD benefits and techniques.
What are some of the advantages of using ESD?
Disección endoscópica de la submucosa
Disección endoscópica de la submucosa
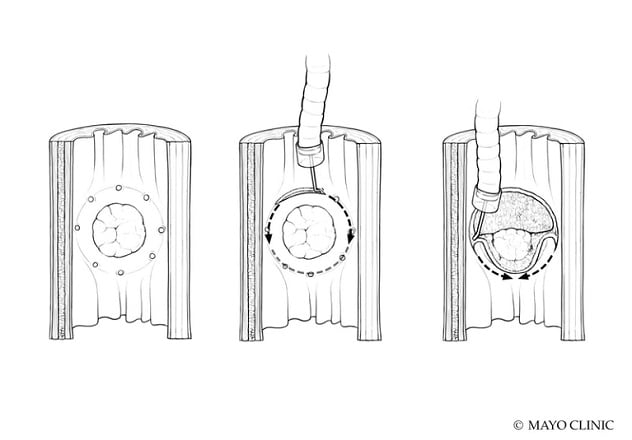
La disección endoscópica de la submucosa es un método muy eficaz para realizar la extirpación en bloque de lesiones demasiado grandes para la resección endoscópica de la mucosa y de aquellas con formas irregulares, incluidas las lesiones multifocales o nodulares. Este tipo de disección consiste en utilizar un bisturí (o bisturíes) específico y una técnica a pulso, que permite a los endoscopistas controlar el tamaño, la forma y la profundidad del tejido resecado.
ESD is a highly effective method for performing en bloc removal of lesions that are too large for EMR and those with irregular shapes, including multifocal or nodular lesions. This approach involves using a dedicated knife (or knives) and a freehand technique, which allows endoscopists to control the size, shape and depth of the tissue resected.
By enabling the removal of a wider area of tissue, ESD can also facilitate improved pathological evaluation and better cancer risk stratification to guide further treatment and surveillance. When used as a cancer resection method, ESD offers more-precise margin determination and is an effective means of achieving negative margin resection for larger and more complex lesions to improve outcomes in patients with cancer.
How do the advantages associated with ESD advance the management of patients with esophageal squamous cell carcinoma or adenocarcinoma?
Imagen previa al procedimiento que muestra un adenocarcinoma esofágico

Imagen previa al procedimiento que muestra un adenocarcinoma esofágico
Se observó una nodularidad de 3 cm dentro de un esófago de Barrett de segmento largo. La biopsia mostró al menos un adenocarcinoma intramucoso.
Imagen postprocedimiento del esófago
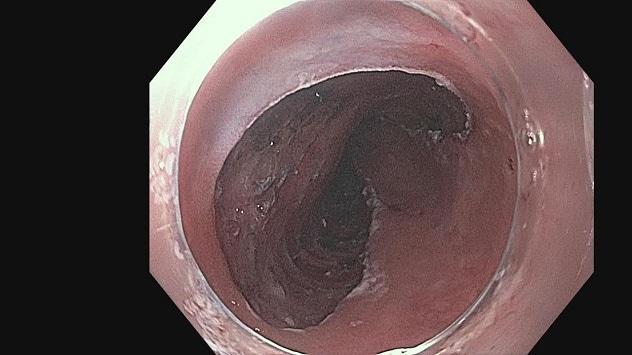
Imagen postprocedimiento del esófago
Durante la disección endoscópica de la submucosa, se extirparon en bloque dos tercios de la circunferencia del nódulo, un total de 5 cm de longitud.
Esophageal squamous cell carcinoma (ESCC) is often found when nodularity is apparent, and at this stage, cancer frequently involves muscularis mucosae or submucosa. Each level of invasion signifies a different level of risk of cancer spread. Endoscopic inspection may not differentiate between minute differences within mucosa. And it may not differentiate between mucosal disease and disease with shallow submucosal (SM) invasion. For risk stratification, ER provides precise pathological staging. ER also aims for curative resection, and thus, negative margin is required. Compared with EMR, ESD offers a more effective way to achieve negative margin resection for curative resection.
Adenocarcinoma arises within Barrett's esophagus or at the gastroesophageal junction and is often accompanied by a wider area of dysplasia. Similar to ESCC, precise staging of superficial cancer is best achieved with pathological evaluation to stratify risks of metastasis and the need for further therapy. Larger resection with ESD facilitates one-piece removal of cancer and dysplasia with negative margins more effectively than does EMR, offering sounder oncologic resection. ESD has been reported to improve subsequent Barrett's eradication therapy.
What is unique about performing ESD in the esophagus?
The esophagus is a tubular organ that can easily be accessed with an upper endoscope. Yet ESD in the esophagus demands a full understanding of anatomy, tools and techniques as well as well-trained skills. SM dissection can be rather effortless because it is aided by the natural angle of approach that is nearly parallel to the esophageal wall. Because the esophagus lacks a protective serosal layer, SM dissection should be performed well above muscularis propria to prevent muscle exposure or injury and reduce adverse events.
Can you describe the two main procedural approaches used during ESD?
The traditional method of ESD involves making a circumferential mucosal incision and completing the SM dissection afterward. An alternate approach, called the tunneling method, involves making the distal and proximal mucosal incisions, dissecting them down to the SM layer, and then completing the SM dissection from the proximal to distal end, creating a tunnel. We typically recommend dissection at the SM2 layer, the middle layer of the SM layer, unless SM invasion of cancer is suspected. General endotracheal anesthesia is used to sustain optimal airway control, respiratory effort and cardiac movement throughout the procedure.
For more information
Fukami, N. Endoscopic submucosal dissection in the esophagus: Indications, techniques, and outcomes. 2023;33:55.
Refer a patient to Mayo Clinic.