概述
肺癌
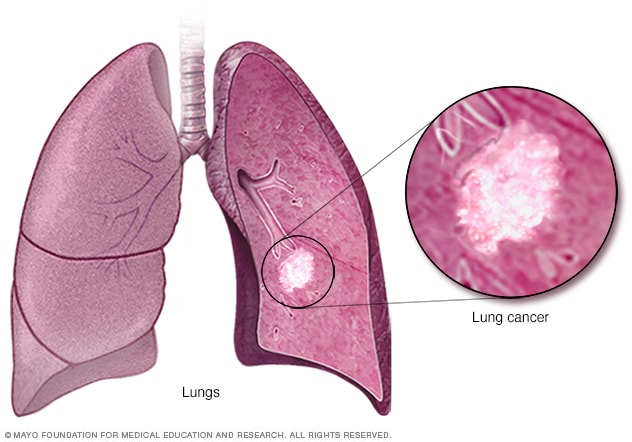
肺癌是一种最开始以肺细胞生长物出现的癌症。肺是胸部两个控制呼吸的海绵质器官。
肺癌是全球癌症死亡的主要原因。
抽烟人群患肺癌的风险最高。患肺癌的风险随着抽烟的时间和数量的增加而增加。即使在抽烟多年后,戒烟也会使您患肺癌的几率也大大降低。从未抽烟的人也可能发生肺癌。
症状
肺癌通常不会在早期引起症状。肺癌的症状通常发生在该病晚期。
发生在肺部及其周围的肺癌体征和症状可能包括:
- 咳嗽不止。
- 胸部疼痛。
- 咳血(即使是少量)。
- 声音嘶哑。
- 气短。
- 哮鸣。
如果肺癌扩散到身体其他部位,可能出现的体征和症状包括:
- 骨痛。
- 头痛。
- 非刻意的体重下降。
- 食欲不振。
- 面部或颈部肿胀。
何时就医
如果出现任何令人担忧的症状,请与医生或其他医疗护理专业人员约诊。
如果您抽烟且一直无法戒烟,请约诊。医疗护理专业人员可以推荐戒烟策略,包括咨询、药物和尼古丁替代产品。
病因
肺癌是肺中细胞的 DNA 发生变化引起的。细胞 DNA 含有指示细胞活动的指令。在健康细胞中,DNA 指令让细胞按设定速度生长和增殖。这些指令会指示细胞在设定的时间死亡。而在癌细胞中,DNA 的变化给出了不同的指令。这些变化会指示癌细胞快速产生更多细胞。在健康细胞应该死亡时,癌细胞仍继续存活。这会导致细胞过多。
这些癌细胞可能会形成一个肿块,称为肿瘤。肿瘤可能生长、侵入并破坏健康的机体组织。随着时间推移,癌细胞可能脱落并扩散至身体其他部位。扩散的癌症被称为转移癌。
抽烟可导致大多数肺癌。在抽烟人群和接触二手烟的人群中均可能会导致肺癌。但肺癌也发生在从不抽烟或接触二手烟的人群中。这些人群的肺癌病因尚不清楚。
抽烟如何导致肺癌
研究人员认为抽烟会损伤覆盖肺部内层的细胞,从而导致肺癌。香烟烟雾中充满致癌物质,称为致癌物。当您吸入香烟烟雾时,致癌物几乎立即导致肺组织发生变化。
一开始身体也许能修复这种损伤。但随着每次反复暴露,覆盖肺部内层的健康细胞的损伤也越来越严重。随着时间推移,这种损伤会导致细胞发生变化,最终可能发展成癌症。
肺癌类型
根据肺癌细胞在显微镜下的外观,将肺癌分为两大类。医疗护理专业人员会基于您所患肺癌的主要类型来决定治疗方案。
肺癌的两大类型包括:
-
小细胞肺癌。小细胞肺癌通常仅发生在抽烟多年的人群中。小细胞肺癌比非小细胞肺癌少见。
-
非小细胞肺癌。非小细胞肺癌包括多种肺癌。非小细胞肺癌包括鳞状细胞癌、腺癌和大细胞癌。
风险因素
很多因素会导致患肺癌的风险升高。有些风险因素可以控制,例如戒烟。其他因素则无法控制,例如家族病史。
导致肺癌的风险因素包括:
抽烟
患肺癌的风险随着日抽烟量的增加而增加。也会随着抽烟年数的增加而增加。无论在哪个年龄段戒烟,均可显著降低出现肺癌的风险。
接触二手烟
即使您不抽烟,如果您周围有人抽烟,你患肺癌的风险也会增加。吸入来自其他抽烟者的烟雾被称为“二手烟”。
曾接受过放射疗法
如果您曾因另一种癌症而接受过胸部放射疗法,您患肺癌的风险可能增加。
接触氡气
氡是土壤、岩石和水中的铀自然分解的一种产物。氡最终会成为您呼吸的空气的一部分。任何建筑物内都可能积聚危险水平的氡气,包括家中。
暴露于致癌物质
在工作场所暴露于致癌物质(称为致癌物)会增加患肺癌的风险。如果您抽烟,风险可能会更高。与肺癌风险相关的致癌物包括石棉、砷、铬和镍。
肺癌家族史
如果父母、兄弟姐妹或孩子患肺癌,则本人患肺癌的风险会更高。
并发症
肺癌可导致多种并发症,例如:
气短
如果肺癌发展到阻塞主要气道,患者可能出现气短。肺癌还可能会导致肺和心脏周围积液。当您吸气时,液体使受累的肺更难完全扩张。
咳血
肺癌可能会导致气道出血。这可能会导致咳血。有时出血会变得很严重。治疗可以控制出血。
疼痛
扩散的晚期肺癌可能会导致疼痛。癌细胞可能会扩散到肺内膜或身体的其他部位,例如骨骼。如果您出现疼痛,请告知医疗护理专业人员。有许多治疗方法可以控制疼痛。
胸腔积液
肺癌可导致胸腔内积聚液体,称为胸腔积液。积液聚集在胸腔内受累肺部周围的空间(即胸膜腔)。
胸腔积液可能引起气短。可以通过治疗将胸腔积液排出。治疗可以降低再次发生胸腔积液的风险。
扩散到身体其他部位的癌症
肺癌经常扩散到身体其他部位。肺癌可能扩散到脑和骨骼。
癌症扩散可能会导致疼痛、恶心、头痛或其他症状,具体取决于受累的器官。一旦肺癌扩散到肺部以外,通常无法治愈。治疗可以减少症状,延长存活时间。
预防
没有确定的方法可以预防肺癌,但如果您做到以下几点便可以降低风险:
不要抽烟
如果您从不抽烟,请不要开始。与孩子谈论不抽烟,让他们了解如何避免这种主要的肺癌风险因素。尽早开始与孩子谈论抽烟的危险,以便他们知道如何应对同侪压力。
戒烟
立即戒烟。即使已经抽烟多年,戒烟也能降低患肺癌的风险。与医疗护理团队讨论可能有助于您戒烟的策略和辅助方法。选项包括尼古丁替代产品、药物和互助组。
避免吸入二手烟
如果您与抽烟的人一起生活或工作,请敦促他们戒烟。至少要让他们在外面抽烟。不去有人抽烟的地方,例如酒吧。寻找无烟的地方。
检测您家中的氡
检查家中氡的水平,尤其是如果您住在已知存在氡问题的地区。可以解决氡水平较高的问题,以使您的家里更安全。氡检测试剂盒通常在五金店销售,也可以在线购买。有关氡检测的更多信息,请联系您当地的公共卫生部门。
避免在工作中使用致癌物
采取预防措施以防止自己在工作中接触有毒化学物质。请遵循雇主规定的预防措施。例如,如果为您提供了保护口罩,请务必佩戴。询问医疗护理专业人员您还能采取哪些措施在工作中保护自己。如果您抽烟,工作场所致癌物造成肺损伤的风险会增加。
摄入富含水果和蔬菜的饮食
选择富含各种水果和蔬菜的健康饮食。食物来源的维生素和营养素是最好的。避免以药丸形式服用大剂量的维生素,因为这可能有害。例如,研究人员希望降低重度抽烟者患肺癌的风险,因此给他们添加了 β 胡萝卜素补充剂。结果表明,补充剂增加了抽烟者患癌症的风险。
每周多日进行锻炼
如果您没有定期运动,请慢慢开始。尽量在每周大多数日子进行锻炼。
Nov. 26, 2024