Overview
Female reproductive system
Female reproductive system
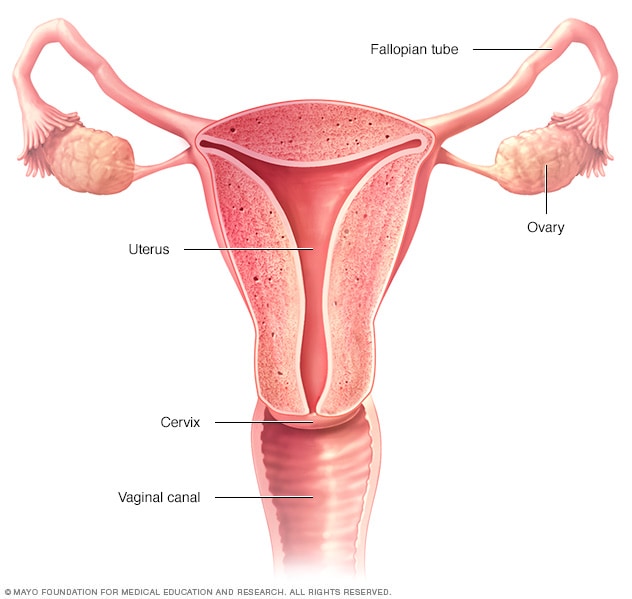
The ovaries, fallopian tubes, uterus, cervix and vagina, also called the vaginal canal, make up the female reproductive system.
Vaginal hysterectomy is a surgical procedure to remove the uterus through the vagina.
During a vaginal hysterectomy, the surgeon frees the uterus from the ovaries, fallopian tubes and upper vagina, as well as from the blood vessels and connective tissue that support it. Then the surgeon removes the uterus.
This approach, which takes the uterus through the vagina, involves a shorter time in the hospital, lower cost and faster recovery than taking the uterus through a cut, called an incision, in the lower belly. But vaginal hysterectomy is not always possible. It depends on the size and shape of the uterus or the reason for the surgery.
Your healthcare professional will talk with you about other types of surgery. These might include hysterectomy using robotic or laparoscopic surgery through small cuts on the belly or a hysterectomy through a longer cut on the belly, called abdominal hysterectomy. Robotic and laparoscopic surgeries most often involve the uterus being removed through the vagina.
Hysterectomy often includes removal of the cervix. This is called a total vaginal hysterectomy. When the surgeon also removes one or both ovaries and fallopian tubes, it's called a total hysterectomy with salpingo-oophorectomy (sal-ping-go-o-of-uh-REK-tuh-me). All these organs are in the pelvis as part of the reproductive system.
Products & Services
Why it’s done
Vaginal hysterectomy treats conditions that affect the female reproductive system, including:
-
Fibroids. Fibroids are tumors in the uterus that aren't cancer. Fibroids can cause bleeding, anemia, pelvic pain, pain during intercourse and bladder pressure.
Large fibroids might need a different type of hysterectomy surgery. The surgery removes the uterus through a cut, called an incision, in the lower belly. This is called an abdominal hysterectomy.
-
Endometriosis. This condition happens when tissue that is similar to the inner lining of the uterus grows outside the uterus. The tissue may grow on the ovaries, fallopian tubes or other organs. Most people with endometriosis have a laparoscopic hysterectomy. For this type of surgery, a surgeon uses a lighted scope with a camera put through a cut in the belly.
Other people with endometriosis might have surgery using robotic controls, called a robotic hysterectomy, or an abdominal hysterectomy. But sometimes a vaginal hysterectomy for endometriosis is possible.
- Adenomyosis. This happens when the tissue that lines the uterus grows into the uterine wall. Adenomyosis makes the uterus get bigger and causes painful, heavy periods. Adenomyosis often goes away after menopause. Or treatment might involve a hysterectomy.
-
Gynecologic cancer. Treatment might involve a hysterectomy for cancer of the uterus, cervix, endometrium or ovaries, or for changes that come before cancer, called precancerous changes. For endometrial cancer, surgeons most often use robotic or laparoscopic hysterectomy.
Treatment for ovarian or cervical cancer most often involves an abdominal hysterectomy. But sometimes a vaginal hysterectomy can treat endometrial or cervical cancer.
- Uterine prolapse. When tissues and ligaments that support the pelvis weaken or stretch out, the uterus can sag into the vagina. This can cause urine leakage, pelvic pressure or trouble passing stool. Removing the uterus and repairing supportive tissues might relieve those symptoms.
- Irregular, heavy or very long periods. A hysterectomy may be needed if medicine or a less invasive surgical procedure doesn't control the bleeding.
- Ongoing, also called chronic, pelvic pain. If a condition of the uterus is the clear cause of pelvic pain, a hysterectomy might help if no other treatment has worked. Chronic pelvic pain can have several causes. So before having a hysterectomy, you need a correct diagnosis of the cause.
For most of these conditions except cancer, hysterectomy may be just one treatment option. Medicines or less invasive gynecological procedures might ease your symptoms.
You cannot become pregnant after a hysterectomy. If you think you might still want to get pregnant, find out about other treatments.
Risks
Although vaginal hysterectomy is mostly safe, any surgery has risks. Risks of vaginal hysterectomy include:
- Heavy bleeding.
- Blood clots in the legs or lungs.
- Infection.
- Damage to other organs.
- Bad reaction to the medicine that puts you in a sleeplike state. The medicine is called anesthesia.
Your surgeon might switch from vaginal hysterectomy to laparoscopic, robotic or abdominal hysterectomy during the surgery if there's a lot of endometriosis or scar tissue.
How you prepare
As with any surgery, people often feel nervous about having a hysterectomy. Here's what you can do to prepare:
- Gather information. Before the surgery, get all the information you need to feel OK about it. Ask your healthcare team any questions you may have.
- Do what your healthcare team tells you about medicines. Find out whether you should take your medicines in the days before your hysterectomy. Be sure your healthcare team knows about all medicines, including those you get without a prescription, dietary supplements or herbal preparations that you take.
- Talk about anesthesia. You might prefer medicine that puts you in a sleeplike state during surgery, called general anesthesia. But blocking feeling in the area of the surgery, called regional anesthesia, might be an option. This also is called spinal block or epidural.
- Arrange for help. It takes time to recover from a vaginal hysterectomy. Ask someone to help you at home for the first week or so.
What you can expect
Talk with your healthcare team about what to expect during and after a vaginal hysterectomy.
During the procedure
You lie on your back, like you do for a Pap test. You might have a tube, called a urinary catheter, put into your urethra to empty your bladder. A member of your surgical team will clean the surgical area with a sterile liquid before surgery.
To do the hysterectomy:
- Your surgeon makes a cut, called an incision, inside the vagina to get to the uterus.
- Using long instruments, your surgeon clamps the uterine blood vessels. Then your surgeon frees the uterus from connective tissue, ovaries and fallopian tubes.
- Your surgeon removes the uterus through the vaginal opening. Stitches that absorb on their own are used to close the incision and control any bleeding inside the pelvis.
The surgeon might cut an enlarged uterus into smaller pieces and remove it in sections. This is called morcellation. The surgeon won't do use this technique if there's a chance of uterine cancer.
Laparoscopic or robotic hysterectomy
Laparoscopically assisted vaginal hysterectomy (LAVH) or robotic hysterectomy may be an option for you. Both procedures allow your surgeon to remove the uterus through the vagina while seeing your pelvic organs through a slender viewing instrument called a laparoscope.
Your surgeon does most of the procedure through small cuts in the belly. The surgeon puts long, thin surgical instruments through the cuts. Your surgeon then removes the uterus through a cut made in your vagina.
Your surgeon might suggest LAVH or robotic hysterectomy if you have scar tissue on your pelvic organs from earlier surgeries or from endometriosis.
After the procedure
After surgery, you're in a recovery room for 1 to 2 hours. Most people go home the day of surgery. Some people need to stay in the hospital overnight.
You take medicine for pain. Your healthcare team will help you get up and move as soon as you can.
You may have bloody vaginal discharge for several days to weeks after a hysterectomy. So you need to wear sanitary pads.
How you'll feel physically
Recovery after vaginal hysterectomy is shorter and less painful than it is after abdominal hysterectomy. A full recovery might take 3 to 4 weeks.
Even if you feel OK, don't lift anything heavier than 15 pounds (6.8 kilograms) for six weeks after surgery. Don't have vaginal sex during that time. But do move around as much as you can. For instance, take short walks.
Contact your healthcare team if pain gets worse. Also call if you have nausea or vomiting or bleeding that's heavier than a menstrual period.
How you'll feel emotionally
After a hysterectomy, you might feel relief because you no longer have heavy bleeding or pelvic pain.
For many people, there's no change in how they respond to sex after hysterectomy. Some who have their ovaries removed may have vaginal dryness and less interest in sex. But some have better sex after hysterectomy. That may be because they no longer have pain during sex.
Some people feel a sense of loss and grief after hysterectomy. They might feel depressed that they can no longer have children. If sadness or painful feelings keep you from enjoying life, talk with a member of your healthcare team.
Results
After a hysterectomy, you no longer have periods. You can't get pregnant.
If you have your ovaries removed before you reach menopause, you'll go into menopause right after surgery. You might have symptoms such as vaginal dryness, hot flashes and night sweats. There are medicines to help manage these symptoms. Your healthcare professional might suggest hormone therapy for menopause even if you don't have symptoms.
If you had periods before your surgery and if you still have your ovaries after surgery, your ovaries keep making hormones and eggs until you reach menopause.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Jan. 11, 2025