Overview
Cardiac ablation

Cardiac ablation
Cardiac ablation is a treatment for irregular heart rhythms, called arrhythmias. It uses thin, flexible tubes called catheters and heat or cold energy to create tiny scars in the heart. The scars block the faulty signals that cause irregular heartbeats. This illustration shows a type of cardiac ablation called pulmonary vein isolation.
Pulmonary vein isolation is a treatment for an irregular heart rhythm called atrial fibrillation (AFib).
It is a type of cardiac ablation. Cardiac ablation uses heat or cold energy to create tiny scars in the heart. The scars block irregular electrical signals and restore a regular heartbeat.
In pulmonary vein isolation, the tiny scars are made in the left upper heart chamber where the four lung veins connect. Those veins are called the pulmonary veins. They bring oxygen-rich blood from the lungs to the heart.
Products & Services
Why it's done
Pulmonary vein isolation is done to reduce the symptoms of atrial fibrillation (AFib). AFib symptoms may include a pounding, fluttering or racing heartbeat, shortness of breath, and weakness. If you have AFib, the treatment may help improve your quality of life.
Pulmonary vein isolation usually is done after you've tried medicines or other treatments first.
Risks
Possible risks of pulmonary vein isolation include:
- Bleeding or infection at the site where the catheter was inserted.
- Blood vessel damage.
- Heart valve damage.
- New or worsening heart rhythm problems, called arrhythmias.
- Slow heart rate, which may need a pacemaker to correct.
- Blood clots in the legs or lungs.
- Stroke or heart attack.
- Narrowing of the veins that carry blood between the lungs and heart, a condition called pulmonary vein stenosis.
- Damage to the tube that connects the mouth and the stomach, called the esophagus, which runs behind the heart.
Talk to your healthcare team about this treatment to understand if it's right for you.
How you prepare
Your healthcare team may do several tests to get more information about your heart health before your cardiac ablation.
You may need to stop eating and drinking the night before your procedure. Your care team gives you instructions on how to prepare.
What you can expect
Before
Pulmonary vein isolation is done in the hospital. A member of your care team places an IV into your forearm or hand and gives you a medicine called a sedative to help you relax.
The amount of sedation needed for the treatment depends on your specific irregular heartbeat and other health conditions. You may be fully awake or lightly sedated. Sometimes a combination of medicines is used to put you in a sleep-like state. This is called general anesthesia.
During
Catheter insertion points for cardiac ablation
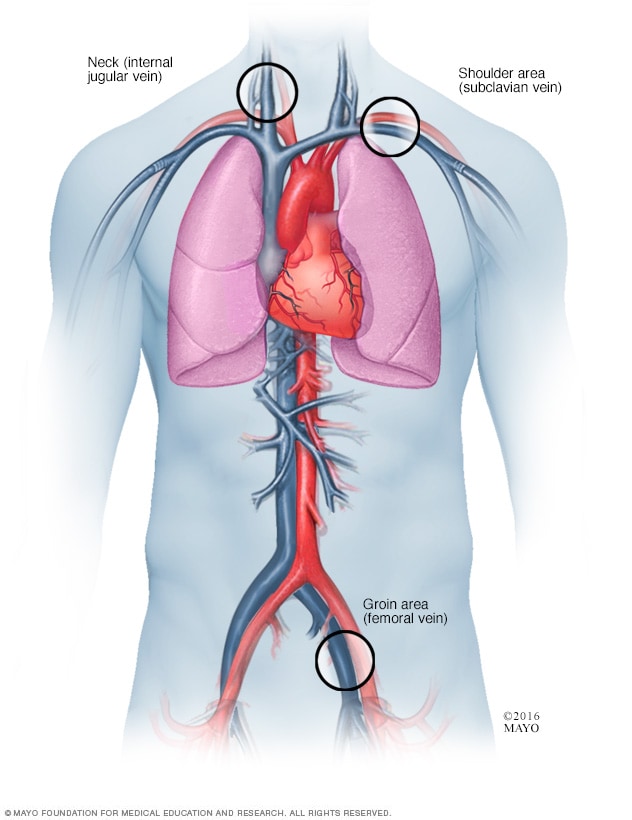
Catheter insertion points for cardiac ablation
During cardiac ablation, a thin, flexible tube called a catheter is passed through a blood vessel to reach the heart. More than one catheter is often used. The catheter may be inserted in the groin, the shoulder or the neck.
During pulmonary vein isolation, the doctor makes a small cut to reach a blood vessel in the groin, shoulder or neck. One or more flexible tubes called catheters are guided through the blood vessel into the area of the heart being treated.
Sometimes dye flows through the catheters. The dye is often called contrast. It helps blood vessels show up more clearly on X-ray images.
Sensors on the tip of the catheters send electrical signals and record the heart's electricity. This part of the procedure is called an electrophysiology (EP) study. An EP study can show where an irregular heartbeat starts in the heart. The information helps your care team know where to apply the treatment.
The doctor guides the catheters into the upper left chamber of the heart where the lung veins connect. One of the following methods is used to create small scars in the heart to block faulty signals:
- Heat energy, called radiofrequency energy.
- Extreme cold energy, called cryoablation.
Usually, each of the four lung veins is treated during pulmonary vein isolation.
You may feel some minor discomfort when the catheter is moved into your heart and when the treatment occurs. If you have severe pain or shortness of breath, let your healthcare team know.
After
Pulmonary vein isolation usually takes 3 to 6 hours to complete. The time may vary depending on the specific irregular heartbeat.
After pulmonary vein isolation, you are typically taken to a recovery area to rest quietly for a few hours. A care professional checks your heartbeat and blood pressure.
Depending on your condition, you may go home the same day or spend the night in the hospital. Plan to have someone else drive you home after your procedure.
You may feel a little sore after your pulmonary vein isolation. The soreness should go away in about a week. Your care team gives you specific information about when you can safely return to any activities.
Results
Most people see improvements in their quality of life after cardiac ablation, including pulmonary vein isolation. But there's a chance that the irregular heartbeat may return. If this happens, you and your care team should talk about your treatment options. Sometimes the pulmonary vein isolation is done again.
Pulmonary vein isolation has not been shown to reduce the risk of a stroke related to AFib. Your healthcare professional may suggest starting or continuing blood-thinning medicines.
Jan. 09, 2024