Prostate cancer screening: Should you get screened?
Making the decision to have prostate cancer screening depends on a variety of factors. Here are some tips that can help you make a good decision.
By Mayo Clinic Staff
Deciding whether to have prostate cancer screening isn't always an easy decision.
Prostate cancer screening can help find prostate cancer early, when treatment is most effective. This seems like a good reason to get screened. But prostate cancer screening isn't perfect. It can lead to more tests and some tests are invasive. Sometimes you have these other tests and they don't find cancer. Sometimes the tests find a cancer that grows slowly and might never actually hurt you. This might lead to cancer treatments that may not have been necessary.
Ultimately, whether to have prostate cancer screening is a decision you make with your healthcare professional. A health professional who understands your health history can help you understand what's best for you based on your risk factors and your personal preferences. Healthcare professionals often call this "shared decision-making."
Here's information to help you get ready to talk with your healthcare professional about prostate cancer screening.
What is prostate cancer screening?
Prostate gland
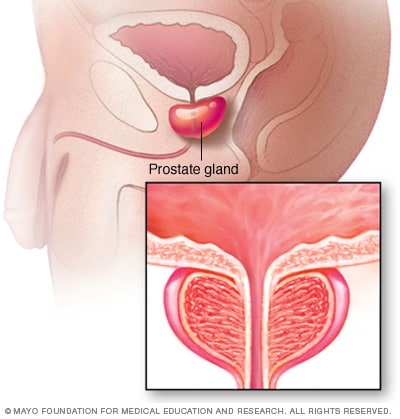
Prostate gland
The prostate gland sits just below the bladder. It surrounds the top part of the tube that drains urine from the bladder, called the urethra. The prostate's main job is to make the fluid that feeds and carries sperm, called seminal fluid. The prostate is part of the male reproductive system.
Prostate cancer screening is testing that looks for prostate cancer in someone who doesn't have any symptoms. The goal is to find prostate cancer when it's small and most likely to be cured.
Prostate cancer is a growth of cells that starts in the prostate. The prostate is a small gland that helps make semen. It's found just below the bladder. The prostate is part of the male reproductive system.
What is the process for prostate cancer screening?
Digital rectal exam
Digital rectal exam
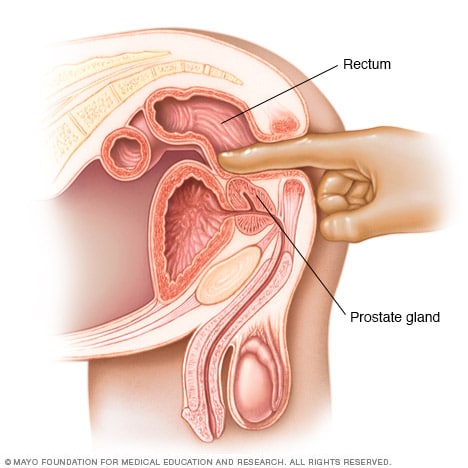
Digital rectal exam
During a digital rectal exam, a healthcare professional inserts a gloved, lubricated finger into the rectum. The health professional feels the prostate gland for anything concerning in the texture, shape or size of the gland.
Prostate cancer screening often involves a blood test. Sometimes it also includes an exam of the prostate by a healthcare professional.
Tests used for prostate cancer screening include:
- PSA test. The prostate-specific antigen blood test, also called a PSA test, uses a sample of blood to look for a protein made by the prostate gland. Typically, there is a small amount of PSA in the bloodstream. If a higher than usual amount is found, it may indicate prostate cancer. If the level of PSA increases quickly from one test to the next, it also may indicate prostate cancer. However, a higher PSA level does not mean that you have prostate cancer.
- Digital rectal exam. During this exam, a healthcare professional inserts a gloved, lubricated finger into the rectum. The prostate is right by the rectum. The health professional feels the prostate for anything concerning in the texture, shape or size of the gland.
These tests may be repeated at regular intervals to watch for any changes over time.
What increases the risk of prostate cancer?
Some people have a greater risk of prostate cancer. They may be more likely to benefit from prostate cancer screening. Knowing the risk factors for prostate cancer can help you determine if or when you want to begin prostate cancer screening. The main risk factors include:
- Older age. After age 50, the chance of having prostate cancer goes up.
- Race. For reasons that aren't well understood, Black people have a higher risk of developing and dying of prostate cancer.
- Family history. Risk is higher among people with a parent, sibling or other close family member with prostate cancer.
- Inherited DNA changes. Certain DNA changes are associated with prostate cancer. Your healthcare team might recommend genetic testing if you have a strong family history of cancer or if a blood relative has been diagnosed with certain DNA changes.
Do experts recommend prostate cancer screening?
Most medical organizations recommend talking with a healthcare professional about the pros and cons of prostate cancer screening. The discussion should include a review of your risk factors and your preferences about screening. For people with an average risk of prostate cancer, experts suggest talking with a healthcare professional about prostate cancer screening around age 50.
For those with an increased risk of prostate cancer, consider talking about prostate cancer screening sooner, around age 40. People with an increased risk include Black people and those with a family history of prostate cancer in a first-degree relative, such as a father or brother. Your healthcare professional can discuss other risk factors with you.
If you choose to have prostate cancer screening, most organizations recommend stopping the screening around age 70 or if you develop other serious medical conditions that limit your life expectancy. However, some people continue with screening beyond age 70 depending on their overall health.
What are the pros and cons of prostate cancer screening?
There are pros and cons to prostate cancer screening.
Benefits of prostate cancer screening include:
- Screening can help detect prostate cancer early. Cancer is easier to treat and is more likely to be cured if it's diagnosed in the early stages of the disease.
- Screening can provide a certain amount of information about your risk. Screening provides more information. Some people want to know their PSA level, even if prostate cancer screening has limitations. If you want to know your PSA level, rather than not know, you might choose screening.
- It may lower the risk of dying of prostate cancer. There is some evidence that screening can lower the number of prostate cancer deaths. But results from studies have been mixed.
Limitations and potential harms to prostate cancer screening include:
- Screening tests aren't foolproof. It's possible for PSA levels to be elevated when cancer isn't present. It's also possible for PSA levels to not be elevated when cancer is present.
- Sometimes screening finds a cancer that isn't likely to hurt you. Not all prostate cancers need treatment. Some prostate cancers are slow growing and never spread beyond the prostate gland. Others grow faster, and treatment can stop them from spreading and becoming life-threatening. Healthcare professionals may not know for sure whether a cancer found during screening needs treatment right away.
- Treatment for prostate cancer may have risks and side effects. These include urinary incontinence, erectile dysfunction or bowel dysfunction.
- The benefits of the test may not outweigh the risks. Prostate cancer screening has lowered the number of prostate cancer deaths, but the number may not be big enough to justify the chances of harm to the person undergoing the testing.
Talk with your healthcare team about the pros and cons of prostate cancer screening. Your care team can help you understand what's best for you. Then you can make a decision about if or when to have prostate cancer screening.
Dec. 17, 2024
- Prostate-specific antigen (PSA) test. National Cancer Institute. https://www.cancer.gov/types/prostate/psa-fact-sheet. Accessed Sept. 28, 2024.
- Prostate cancer early detection. National Comprehensive Cancer Network. https://www.nccn.org/guidelines/guidelines-detail?category=2&id=1460. Accessed June 25, 2024.
- Grossman DC, et al. Screening for prostate cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018; doi:10.1001/jama.2018.3710.
- Wei JT, et al. Early detection of prostate cancer: AUA/SUO guideline part I: Prostate cancer screening. The Journal of Urology. 2023; doi:10.1097/JU.0000000000003491.
- Wei JT, et al. Early detection of prostate cancer: AUA/SUO guideline part II: Considerations for a prostate biopsy. The Journal of Urology. 2023; doi:10.1097/JU.0000000000003492.
- Pinsky PF, et al. Screening for prostate cancer. New England Journal of Medicine. 2023; doi:10.1056/NEJMcp2209151.
- Prostate cancer screening (PDQ) — Patient version. National Cancer Institute. https://www.cancer.gov/types/prostate/patient/prostate-screening-pdq. Accessed Oct. 2, 2024.
- AskMayoExpert. Prostate cancer: Screening (adult). Mayo Clinic; 2023.
- Medical review (expert opinion). Mayo Clinic. Oct. 15, 2024.