Overview
Atrial fibrillation ablation is a treatment for an irregular and often very fast heartbeat called atrial fibrillation (AFib). The treatment uses heat or cold energy to create tiny scars in an area of the heart. The signals that tell the heart to beat can't pass through scar tissue. So the treatment helps block faulty signals that cause AFib.
Atrial fibrillation ablation may be done if medicines or other treatments for AFib don't work. But sometimes it's the first treatment for certain people with AFib.
A doctor most often uses thin, flexible tubes called catheters to do atrial fibrillation ablation. The tubes are placed into blood vessels and guided to the heart. Less commonly, ablation is done during heart surgery.
Types
Why it's done
Atrial fibrillation

Atrial fibrillation
In a typical heart, a tiny group of cells at the sinus node sends out an electrical signal. The signal travels through the heart's upper chambers to the atrioventricular (AV) node. The signal then passes into the lower heart chambers, causing them to squeeze and pump out blood. In atrial fibrillation, electrical signals fire from many locations in the upper chambers, causing them to beat chaotically. Since the AV node doesn't prevent all of these chaotic signals from entering the lower chambers, the heart beats faster and irregularly.
Atrial fibrillation ablation is done to fix and prevent an irregular and often very fast type of heartbeat called AFib. You may need this treatment if you have a fast, fluttering heartbeat that doesn't get better with medicine or other treatments.
Risks
Possible atrial fibrillation ablation risks include:
- Bleeding or infection at the area where the catheters were placed.
- Blood vessel damage.
- Heart valve damage.
- New or worsening irregular heartbeats, called arrhythmias.
- Slow heart rate that could require a pacemaker to fix.
- Blood clots in the legs or lungs.
- Stroke or heart attack.
- Narrowing of the veins that carry blood between the lungs and heart, called pulmonary vein stenosis.
- Damage to the kidneys from dye, called contrast, used to see the arteries during the treatment.
Talk to your healthcare professional about the risks and benefits of atrial fibrillation ablation. Together you can decide whether the treatment is right for you.
How you prepare
You may have several tests to check your heart health.
Your healthcare team tells you how to prepare for atrial fibrillation ablation.
- You usually need to stop eating and drinking the night before the treatment.
- Tell your care team about all the medicines you take. The team tells you how or if you should take them before the treatment.
What you can expect
Before
Atrial fibrillation ablation is done in a hospital. A member of your care team places an IV into your forearm or hand. You usually get medicines to help you relax. This is called sedation.
The amount of sedation needed for the treatment depends on the type of irregular heartbeat you have and your overall health. You may be fully awake or lightly sedated. Some people get a combination of medicines to put them in a sleep-like state. This is called general anesthesia.
During
Catheter insertion points for cardiac ablation
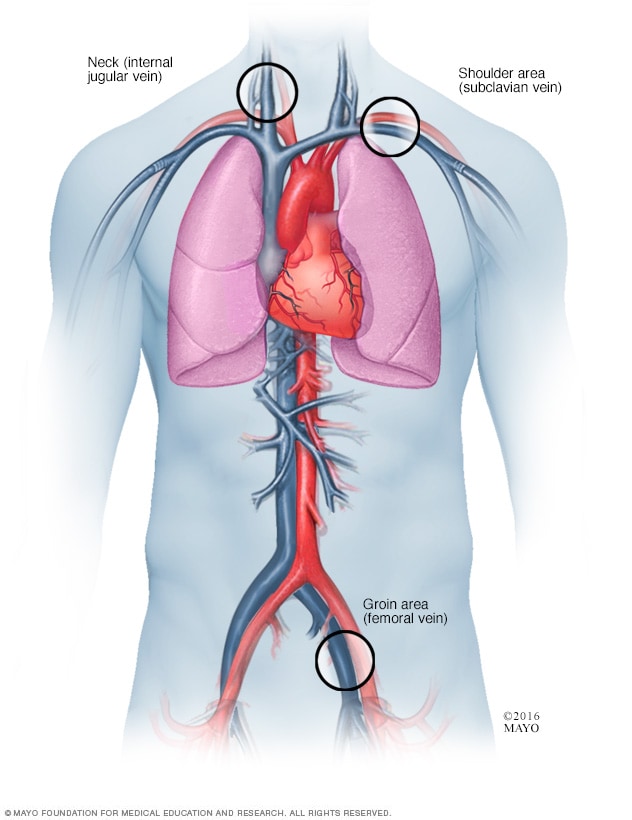
Catheter insertion points for cardiac ablation
During cardiac ablation, a thin, flexible tube called a catheter is passed through a blood vessel to reach the heart. More than one catheter is often used. The catheter may be inserted in the groin, the shoulder or the neck.
What happens during atrial fibrillation ablation depends on the specific treatment being done.
Most often, a doctor inserts one or more thin, flexible tubes called catheters into a blood vessel and guides them to the heart. These tubes are usually placed in a blood vessel in the groin, shoulder or neck.
Dye called contrast flows through the tube. The dye helps blood vessels show up more clearly on X-ray images.
The doctor uses one of the following ablation methods to create small scars in the heart. The scars block the irregular heartbeats:
- Heat energy, called radiofrequency energy.
- Extreme cold, called cryoablation.
You shouldn't feel any discomfort during the procedure. If you have bad pain or shortness of breath, tell your care team.
Atrial fibrillation ablation usually takes 3 to 6 hours. Complicated procedures may take longer. For example, if you have a type of atrial fibrillation ablation called AV node ablation, you need a permanent pacemaker to control your heart rate. The pacemaker may be placed before or during the ablation.
Another type of ablation to treat AFib is called the maze procedure. This type of ablation is done during open-heart surgery. The surgeon creates a pattern of scar tissue in the heart using a scalpel or device that delivers heat energy. The scars block irregular heart signals that cause atrial fibrillation.
After
After the procedure, you rest in a recovery area for a few hours. A care team closely checks on you. Depending on your condition, you may go home the same day or spend the night in the hospital. Plan to have someone drive you home.
Some people feel sore after atrial fibrillation ablation. The soreness shouldn't last more than a week. Most people can return to their daily activities within a few days. But ask your care team what activities are safe for you. In general, avoid heavy lifting for about a week.
Results
Most people see improvements in their quality of life after atrial fibrillation ablation. But there's a chance that AFib may return. If this happens, another ablation may be done or your healthcare professional might suggest other treatments.
AFib is linked to stroke. Atrial fibrillation ablation hasn't been shown to reduce this risk. After ablation, you may need to take blood thinners to reduce your stroke risk.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.