Oct. 01, 2024
New technologies now available for use at the scene of an injury and at your trauma center enable a one-step airway maneuver by any professional with brief training and a video recording of all laryngoscopies.
Advanced supraglottic airway device
 Advanced supraglottic airway device
Advanced supraglottic airway device
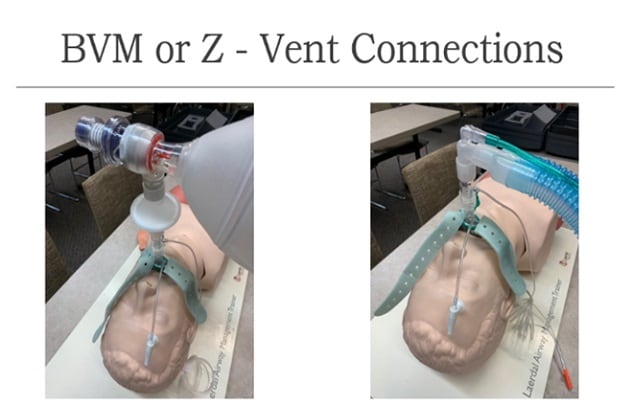
A manikin in a Mayo Clinic simulation center allows healthcare professionals to practice supraglottic airway insertion.
(Photo by Todd Dorn, Mayo Clinic paramedic)
A second-generation supraglottic airway device enables first responders to secure the injured patient's airway when endotracheal intubation is not the best option. The supraglottic airway device is designed with a thermoplastic elastomer and includes a noninflatable cuff with a gel-like substance moldable to the patient's anatomy. This airway device includes a buccal cavity antirotation stabilizer, epiglottic ridge, gastric channel, insertion depth guide and integrated bite block.
"This advanced supraglottic airway device is fast and easy, allowing first responders to get control of the injury sooner. For critical trauma patients, minutes or even seconds can make the difference between life and death."
According to a Journal of Anaesthesiology Clinical Pharmacology publication and Aaron B. Klassen, M.D., M.A., associate medical director for clinical practice for Mayo Clinic Ambulance Service at Mayo Clinic in Minnesota, the advanced supraglottic airway device offers these benefits:
- Simple. It requires a one-step airway maneuver, and any first responder with minimal training — including police and firefighters — can insert it. Its ease of use by a variety of professionals contrasts with the challenges of inserting an endotracheal tube and the limited list of potential users.
- Not allergenic. The device prevents common allergic reactions due to its latex-and PVC-free composition.
- Flexible. When warmed by the patient's body, the device is pliable and moldable.
- Fast. If trained, any first responder can supply air to the patient's trachea even before an ambulance arrives. This reduces risk due to lack of oxygenation and ventilation and reduces time at the scene of an injury, accelerating the patient's arrival at a trauma center.
- Sufficient seal. While this device does not offer an endotracheal tube-equivalent seal, it provides an adequate seal for securing an airway that is often superior to a seal with a face mask.
Dr. Klassen considers this device a potential lifesaver for patients experiencing traumatic injuries.
"This advanced supraglottic airway device is fast and easy, allowing first responders to get control of the airway sooner," says Dr. Klassen. "For critical trauma patients, minutes or even seconds can make the difference between life and death. We want to reduce time in the field and get injured patients to the operating room and stability sooner."
Video laryngoscopy system
 Video laryngoscopy system
Video laryngoscopy system
A paramedic demonstrates the use of a video laryngoscopy system.
(Photo by Todd Dorn, Mayo Clinic paramedic)
Another device now available for trauma care is the video laryngoscopy system, which provides a visual recording of all intubation attempts. This facilitates learning and improving future laryngoscopy.
The use of a video laryngoscope is rapidly replacing the use of standard laryngoscopes in the prehospital environment. The use of this device rather than a standard laryngoscope has these benefits:
- Portability. The video laryngoscope is a compact, portable, hand-held device. The screen and multiple laryngoscope blades can be carried in a case the size of a small laptop bag.
- Postprocedural viewing. This device visually records the entire intubation attempt from the camera view of the laryngoscope. Postprocedural viewing provides ambulance leadership and crew members with an opportunity to watch the procedure later to identify aspects performed well and those the crew could improve in the future. Quality improvement specialists receive the videos taken, collect data and write up an initial review. The specialist sends the video and the written feedback to the ambulance service medical director for review, who then sends the information to the ambulance crew members.
"Previously, feedback for ambulance crew members was based on their own documentation," says Dr. Klassen. "However, having performed the procedure themselves, they might not know if something was overlooked. The quality improvement specialist and the medical director may observe things that the crew didn't notice at the time. We've learned helpful things through these videos."
Dr. Klassen says the laryngoscopy video offers the opportunity to identify techniques that could or should have been used in the procedure. It also may reveal training gaps if ambulance leadership notes a pattern of crew members making similar mistakes. For instance, the video may show that the blade's position was less than ideal during the procedure.
He also sees the opportunity for emergency department professionals to use the video laryngoscopy for educational purposes.
Dr. Klassen strongly encourages trauma centers and ambulance services that use a laryngoscope to switch to a video laryngoscopy system. If your trauma center has one, he recommends familiarizing yourself with it so that when an injured patient presents with a potential laryngeal injury, you understand the device and can troubleshoot if any issues arise.
For more information
Jadhav PA, et al. I-gel versus laryngeal mask airway-Proseal: Comparison of two supraglottic airway devices in short surgical procedures. Journal of Anaesthesiology Clinical Pharmacology. 2015;31:221.
Refer a patient to Mayo Clinic.