Oct. 14, 2022
Overall, rhabdomyosarcoma affects only about 350 children a year in the U.S. Some subtypes of the disease have a 70% survival after treatment. Other subtypes have worse prognoses. And if the disease recurs, mortality is high. For those reasons, it's imperative to get the right care right away.
Candace F. Granberg, M.D., a pediatric urologist in Urology at Mayo Clinic in Rochester, Minnesota, along with a multidisciplinary surgical team, has operated on several children with rhabdomyosarcoma. Approximately 20% of pediatric rhabdomyosarcoma cases are genitourologic, and some require complex surgery.
"Rare cancers need rare cancer surgery by a team that does it often and well," says Dr. Granberg. "For this particular cancer, which is unforgiving, you get one good shot. You must have negative margins after surgery — confirmed by pathologists examining tissue in the frozen section pathology lab during surgery — with no cancer cells left behind. If that's not the case, there is a much higher chance that the cancer will recur."
Dr. Granberg and her surgical partner, Patricio C. Gargollo, M.D., a pediatric urologist at Mayo Clinic in Rochester, Minnesota, see pediatric patients with primary and recurrent rhabdomyosarcoma. Through a clinical trial, Mayo Clinic offers a cutting-edge treatment option that combines surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) to treat relapsed intra-abdominal and pelvic rhabdomyosarcoma.
In this process, surgeons remove all visible tumors and apply heated chemotherapy into the patient's abdomen. Unlike systemic chemotherapy, HIPEC delivers the agents directly to any remaining cancer cells in the abdomen. It's hypothesized that heating the solution may improve drug absorption.
According to Carola A S. Arndt, M.D., a pediatric hematologist and oncologist at Mayo Clinic in Rochester, Minnesota, the chemotherapy agents to treat rhabdomyosarcoma remain largely unchanged since the 1970s. HIPEC is an experimental therapy used to attempt to eradicate microscopic cancer cells that may remain behind after surgery.
Dr. Granberg says parents also appreciate that Mayo Clinic is studying these cancers so other children's lives can be spared. Research teams at Mayo Clinic preserve patients' tissue, blood and cells in a biobank. Mayo Clinic researchers also are running several studies to better characterize these rare tumors and so that they can study the tumors and identify new therapeutic targets.
Riley's story
At age 8, Riley Kane was diagnosed with pediatric rhabdomyosarcoma. His primary care provider noticed a lump above his testicle, and a specialist referred the family to Children's Minnesota. Surgeons removed Riley's tumor, and a biopsy revealed that the tumor was a rare form of cancer.
3D modeling
3D modeling
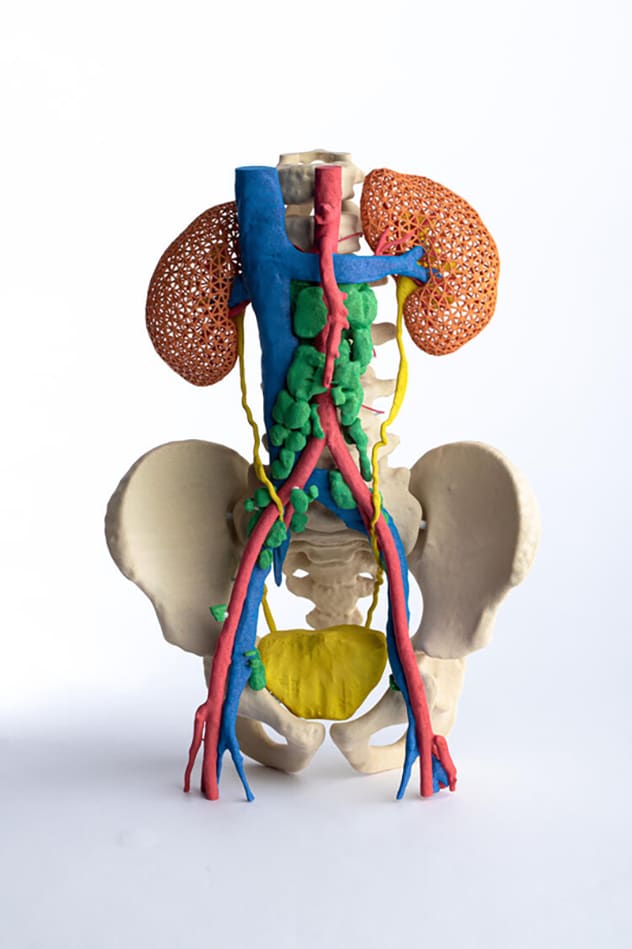
Mayo Clinic's pediatric solid tumor team met with pediatric patient Riley Kane's oncologist virtually and used 3D modeling to plan his surgery.
Dr. Granberg met with the family to discuss a care plan for Riley. Additional imaging showed that his cancer was advanced and had spread to lymph nodes in his abdomen. A medical team led by Jonathan M. Morris, M.D., a radiologist at Mayo Clinic in Rochester, Minnesota, used a model of Riley's anatomy to guide his surgical team.
In March 2021, the Mayo Clinic team led by Dr. Granberg and Stephen A. Boorjian, M.D., a urologist and the chair of Urology, removed 150 lymph nodes in an eight-hour procedure. During this procedure, the surgeons placed a port for chemotherapy and removed a small portion of Riley's other testicle to freeze for fertility preservation.
While at Mayo Clinic, Riley commenced 42 weeks of chemotherapy under the direction of Wendy A. Allen-Rhoades, M.D., Ph.D., a pediatric oncologist and hematologist at Mayo Clinic in Rochester, Minnesota, who collaborated with his physicians at Children's Minnesota. Two months later, Riley began the first of 30 doses of daily proton beam therapy.
The family traveled from home in Rogers, Minnesota, to Rochester — 110 miles each way — Monday through Friday for six weeks for proton beam therapy. Riley had most of his chemotherapy close to home at Children's Minnesota. He finished treatment at the end of 2021. At a checkup in January, his scans were clear, showing no evidence of cancer. Riley will continue to be checked every few months for now and throughout his life for secondary effects of radiation therapy.
"Parents will go to the ends of the earth to save their children," says Dr. Granberg. "We're glad to be the destination for pediatric rhabdomyosarcoma treatment. We'll be glad when no parent has to struggle to find the right team to treat their child and cure their cancer."
For more information
Based on One good shot: Rare expertise for rare pediatric cancer. Mayo Clinic Alumni. 2022;2:18.
Refer a patient to Mayo Clinic.