Jan. 31, 2020
Since the 1970s, there's been little or no change in the overall survival of patients with very high-risk rhabdomyosarcoma, according to a study in the July 2018 issue of Cancer Treatment Reviews co-authored by Carola A S. Arndt, M.D., a pediatric oncologist at Mayo Clinic Children's Center in Rochester, Minnesota.
For that reason, specialists at Mayo Clinic Children's Center are approaching treatment as a multidisciplinary team, offering cutting-edge treatments and research to improve the outcomes of children with rhabdomyosarcoma.
"We are blessed at Mayo Clinic to have an amazing team of people who are dedicated, talented and well versed in sarcoma surgery to give these kids the best chance at beating this rare cancer," says Patricio C. Gargollo, M.D., a pediatric urologist at Mayo Clinic Children's Center.
Specialists and subspecialists, including pediatric urologists, pediatric surgeons, orthopedic oncology surgeons, and radiation oncologists work together to create personalized, targeted surgical and radiation therapy plans for each child.
Hyperthermic intraperitoneal chemotherapy allows for direct administration
Hyperthermic intraperitoneal chemotherapy (HIPEC) setup
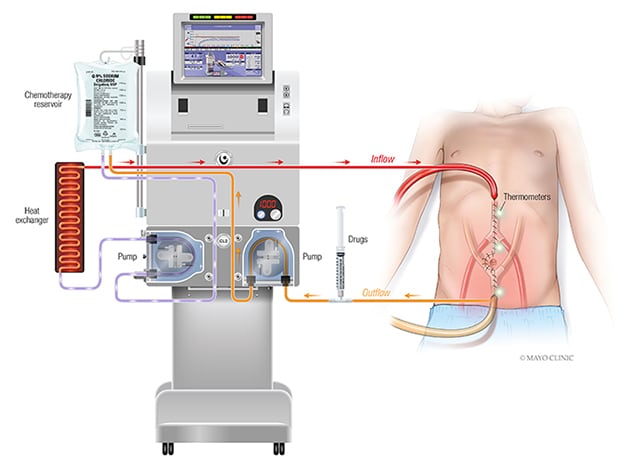
Hyperthermic intraperitoneal chemotherapy (HIPEC) setup
Hyperthermic intraperitoneal chemotherapy (HIPEC) involves administration of a highly concentrated, heated chemotherapy solution directly into the abdomen intraoperatively after complete removal of all visible tumor.
One innovative and unique component of sarcoma care at Mayo Clinic includes hyperthermic intraperitoneal chemotherapy (HIPEC), one of only a few programs available in the country. HIPEC is a highly concentrated, heated chemotherapy solution administered directly into the abdomen during surgery, targeting any remaining cancer cells.
Proton beam therapy spares vital organs, healthy tissue
Mayo Clinic's Proton Beam Therapy Program uses pencil beam scanning, which allows oncologists to deliver higher doses of radiation to cancer cells while sparing heathy tissue. This targeted therapy is ideal for children with tumors close to vital organs that are still developing.
3D models enable surgeons, families to better understand tumor
Using data from a child's MRI or CT scan, pediatric radiologists create 3D models of the tumor. Models are brought into the operating room for reference during surgery, enabling surgeons to see exactly where to cut to remove the entire tumor or where radiation is needed. Parents also can see the model before surgery to gain a better understanding of their child's tumor.
Care that continues at home
Mayo specialists work together to ensure that care continues even when the patient goes home. "We work closely with the home oncologist or home primary care physician to coordinate care as appropriate," says Dr. Arndt. "This may be a continuation of chemotherapy with the home oncologist or support after chemotherapy."
For more information
Arndt CAS, et al. Fifty years of rhabdomyosarcoma studies on both sides of the pond and lessons learned. Cancer Treatment Reviews. 2018;68:94.
Proton Beam Therapy Program. Mayo Clinic.