March 27, 2020
Mayo Clinic is investigating infrapatellar saphenous nerve neuroma as a source of pain after total knee arthroplasty. About 20% of patients who have a total knee arthroplasty are dissatisfied with the result, often due to residual pain. Mayo Clinic's work seeks to address persistent medial knee pain that lacks a clear etiology, such as infection, misalignment or loosening of the prosthesis.
"This type of medial pain can be misdiagnosed as tendonitis or pes anserine bursitis. But it often turns out to be an infrapatellar saphenous nerve neuroma that is causing pain," says Glenn G. Shi, M.D., an orthopedic surgeon at Mayo Clinic in Jacksonville, Florida. "Patients who have a misdiagnosis might be sent to pain clinics or physical therapy with no reasonable outcomes. That leads to a lot of frustration for patients and orthopedic surgeons alike."
The incidence of infrapatellar saphenous nerve neuroma after total knee replacement is unknown. "But we think this problem is underrecognized," Dr. Shi says.
Infrapatellar branch of the saphenous nerve
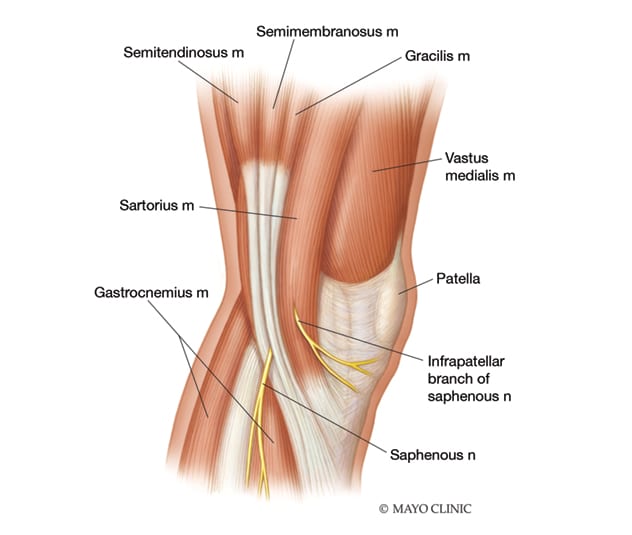
Infrapatellar branch of the saphenous nerve
Illustration shows the infrapatellar branch of the saphenous nerve, which is typically severed during total knee arthroplasty.
In cadaveric studies, Mayo Clinic has found that the standard surgical incision used in total knee arthroplasty almost always severs the infrapatellar saphenous nerve. The severed nerve generally doesn't affect the knee's function. But the nerve ending can become trapped in the incision's closure or in subsequent scar tissue, leading to a neuroma.
"Why some people get a neuroma and others don't is part of our investigation," Dr. Shi says. "We are also trying to determine if we can somehow tuck the nerve end into the knee during surgery, to protect it from entrapment and prevent problems down the road."
Seeking a modified surgical technique
Mayo Clinic's investigation of saphenous nerve neuroma after total knee arthroplasty encompasses several studies. The cadaveric project aims not only to understand the anatomical pattern of the nerve's intersection with a standard knee-replacement incision but also to investigate suturing techniques that avoid trapping the nerve in the incision closure. Clinical studies assess how frequently orthopedic surgeons see the saphenous nerve during standard total knee arthroplasty. "If we can teach our orthopedic surgeons to see the nerve, we can potentially avoid injury that might require another surgery," Dr. Shi says.
In addition, Mayo Clinic is investigating strategies to treat infrapatellar saphenous nerve neuroma. One approach involves ultrasound-guided hydrodissection of the nerve from the adjacent interfascial planes, followed by a corticosteroid injection. A preliminary Mayo Clinic study found that this minimally invasive procedure significantly reduced medial knee pain for nine of 16 patients studied.
For patients whose pain persists after hydrodissection, Mayo Clinic is exploring options for surgical repair. "We are trying to use a less invasive incision to find the nerve end and place it in an area where it is protected from scar tissue," Dr. Shi says. A prospective study is using a similar approach during total knee arthroplasty to prevent infrapatellar saphenous nerve neuroma from developing.
"This problem isn't widely discussed among orthopedic surgeons, but it's very impactful. Up to 3 million people are expected to have total knee arthroplasty by 2035," Dr. Shi says. "Our goal is to bring attention to this problem, which we think contributes to patients' dissatisfaction after total knee arthroplasty. A modified technique for the procedure can potentially avoid the development of neuroma and reduce pain."