Sept. 23, 2022
Orthopedic surgeons at Mayo Clinic in Florida are now performing osseointegration, a technique to attach a prosthesis directly to bone, making it easier for patients to use with short residual limbs following an amputation. They are using the first Food and Drug Administration (FDA)-approved osseointegration implant in the United States. This procedure has been performed previously at a military facility, Walter Reed Army Medical Center, and is now available for the civilian population.
"In certain cases, the residual limb is too short for a traditional socket-style prosthesis," says Benjamin K. Wilke, M.D., an orthopedic surgeon at Mayo Clinic in Florida. "These are usually very high amputations. Typical prosthetics need enough surface area for the socket to hold. They can get good suction and seal with below-knee amputations. However, if amputations are close to the hip, it becomes more challenging."
Brief osseointegration history at Mayo Clinic and worldwide
In May 2021, orthopedists at Mayo Clinic in Florida performed the first osseointegration for a patient who lost a leg to cancer. The patient now ambulates with one crutch and is working with a physical therapist to remove all gait aids. A second patient recently completed stage 2 of the two-stage procedure, and a third patient completed stage 1. Dr. Wilke says patients with high above-knee amputations appropriate for osseointegration often have required limb removal following cancerous tumors or other diseases, or irreparable or life-threatening damage from traumatic incidents such as motor vehicle crashes.
Osseointegration arose from efforts in Europe to find solutions for patients who failed traditional sockets used for prosthetic devices. Surgeons in Europe, says Dr. Wilke, have more experience with the procedure than do surgeons in the United States. Osseointegration arrived stateside mostly for blast injury use at Walter Reed. Dr. Wilke says osseointegration now is spreading to U.S. academic medical centers, predicting it will become commonplace in 5 to 10 years.
Mayo Clinic orthopedic surgeons formed a unique relationship with a physiatrist at Brooks Rehabilitation Hospital to whom they'd refer patients post-amputation. Dr. Wilke, Mayo colleagues and the Brooks physiatrist considered potential techniques to improve fastening and prosthesis use for patients with high-leg amputations. This collaboration continues today with osseointegration at Mayo Clinic in Florida then referral to Brooks for rehabilitation.
How osseointegration works
Stages of osseointegration
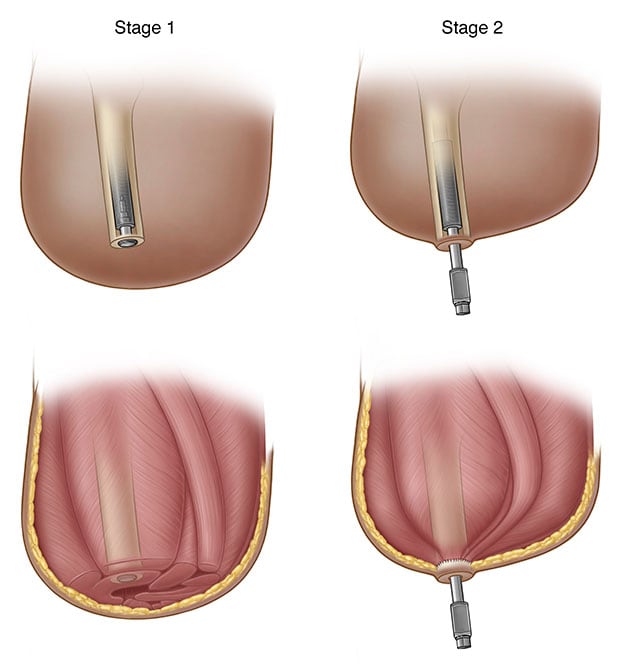
Stages of osseointegration
The process of osseointegration in stages for patients with short residual limbs post-amputation.
Osseointegration is a unique method to connect prosthetics and residual limbs, removing the socket. The surgery begins with screw implantation. After 6 weeks to 3 months of healing, the orthopedist performs the second surgery, inserting the abutment to which the prosthetic limb will attach. Plastic surgery teams assist during this procedure with flap development.
There is a risk of infection with osseointegration. Infections are usually mild and require oral antibiotics for 1 to 2 weeks. Osseointegration includes built-in safety features. If patients fall post-procedure, they can hypothetically fracture the remaining bone. But the technology includes a torque limiter that is designed to limit the force on the bone. If patients fall down the stairs, hitting with significant force, the prosthetic is designed to break away, similar to skis when skiers crash.
Dr. Wilke considers Mayo Clinic in Florida's osseointegration practice distinct in its coordinated team effort, with strong relationships between Mayo orthopedic and plastic surgeons, and with the rehabilitation hospital physiatrist, along with a significant support structure.
Though osseointegration is possible for many with near-hip amputations, contraindications include severe diabetes, vascular issues and infection, the last of which historically has been challenging with amputations. Osseointegration also is inappropriate for long residual limbs post-amputation, as it would require bone removal to avoid knee imbalance.
Dr. Wilke's early observations on osseointegration
Dr. Wilke is excited about what osseointegration provides for eligible patients.
"The patients have significantly better mobilization," he says. "One patient is able to do walks up and down ramps almost like someone without a prosthetic. The gait is much closer to someone's gait unaffected by amputation — better than with suction-based prosthetics. The energy expended to walk is also less."
With osseointegration, patients also have significant prosthetic sensory abilities Dr. Wilke finds intriguing.
"Sensory receptors in the bone allow patients to close their eyes standing on tile, move their legs and tell when the prosthetic foot slides between two tiles," he says.
Though initial osseointegration costs more than a socket, Dr. Wilke anticipates the procedure's cost over time will be lower. The cost savings will be realized from fewer needed prosthetic modifications.
Mayo Clinic in Florida osseointegration practice and patient referrals
Because osseointegration is not offered everywhere, yet useful for patients with high above-knee amputations, Dr. Wilke anticipates self-referrals. He also welcomes referrals from physicians whose patients would benefit from the procedure.
He suggests allowing patients with high above-knee amputations to heal, then sending them to Mayo Clinic in Florida for osseointegration quickly, rather than referring them years later.
"This is new and exciting for the amputee world," says Dr. Wilke. "We want to help these patients experience as high a quality of life as possible with prosthetics that allow them to participate in activities meaningful to them."
For more information
Refer a patient to Mayo Clinic.