Sept. 23, 2022
The proposition of total knee arthroplasty (TKA) or total hip arthroplasty (THA) for a patient with morbid obesity — an individual with a body mass index (BMI) of 40 or greater — requires careful risk and benefit assessment by the orthopedic surgeon and the patient, according to Nicholas A. Bedard, M.D., an orthopedic surgeon at Mayo Clinic's campus in Rochester, Minnesota.
"As BMI goes up, so does risk of complications," he says. "The risks start to increase exponentially at a BMI of 40."
He says even for patients with a BMI of 30, risk level increases slightly compared with that of patients who have a BMI under 30.
Potential risks and challenges for patients with 40-plus BMI
Knee implant
Knee implant
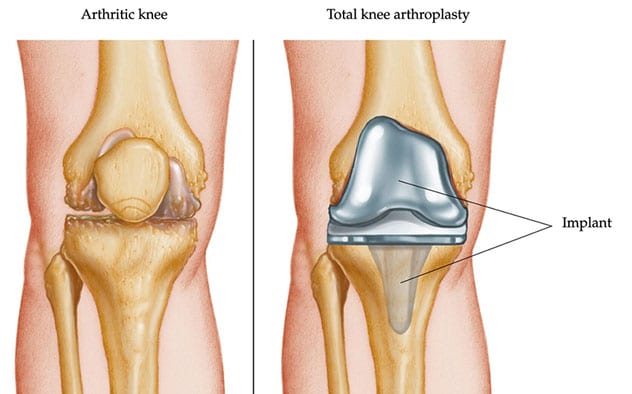
An arthritic knee and repair with total knee arthroplasty
Total hip arthroplasty

Total hip arthroplasty
Total hip arthroplasty for a patient with morbid obesity
BMI is independently associated with increased risk of postoperative complications after THA and TKA, says Dr. Bedard. He also indicates obesity usually does not occur in a vacuum, without other health consequences. In fact, it can be a marker of poor overall wellness: Individuals who have a 40-plus BMI tend to be overall less healthy, and often have other medical problems that can increase their risk of complications.
Potential risks and challenges for performing a TKA or THA for a patient with morbid obesity include:
- Soft tissue depth, which makes implant positioning more difficult for the surgeon
- Increased risk of wound complications
- Elevated infection risk
- Increased risk of THA dislocation due to soft tissue impingement or tissue levering the joint out of place
Dr. Bedard says infection after TKA and THA is a significant risk for patients with 40-plus BMI, often leading to one or two additional surgeries and worse function.
Yet, despite greatly increased TKA or THA risks and challenges for those with morbid obesity, these patients are still debilitated by arthritis, and the need persists to help them.
"It's hard to deny someone a procedure just based on BMI cutoff," says Dr. Bedard, considering the example of a patient who has a BMI of 52 and who smokes cigarettes and has diabetes, and how additional comorbidities like these compound each other. "We work with them individually to modify their risk factors to improve the likelihood of getting them through surgery safely."
According to Dr. Bedard, patients with morbid obesity who do not experience any complications post-TKA or post-THA do as well as patients with lower BMI after surgery, experiencing good outcomes, including decreased pain and improved function.
"Patients with morbid obesity can have similar functional increases after TKA or THA as patients with lower BMI who have the surgery," says Dr. Bedard. "The vast majority get through surgery successfully. The main difference is comparative risk, which can be 2 to 5 times higher than that of patients who have lower BMI."
He acknowledges, however, that regardless of BMI, no surgery is risk-free.
"Every surgery has risk," he says. "You have to work with the patient to say, 'What's an acceptable risk to you?'"
While Dr. Bedard emphasizes that determination of unacceptable risk level is an individual decision, for some patients needing TKA or THA, the pain level they are experiencing makes decision-making difficult. In this case, Dr. Bedard suggests the surgeon help guide them in a shared decision-making process.
Mayo Clinic's approach to helping individuals with high BMI who need TKA or THA
What Dr. Bedard recommends, in light of risks for the patient with high BMI who needs pain alleviation and functional improvement, is optimizing the patient's weight and health pre-surgery. This typically includes the following process with a surgeon, patient and other physicians who specialize in weight loss:
- Discussing the patient's arthroplasty risks and any patient concerns
- Setting reasonably attainable health improvement goals
- Presenting options for how to reach the goals and pros and cons of each potential tool
Dr. Bedard emphasizes compassion and a can-do attitude with patients in this situation, as many have been denied surgery elsewhere.
Mayo Clinic's BMI targets for TKA and THA are not different from those of other institutions. The distinction for Mayo Clinic lies in a multidisciplinary approach. Mayo Clinic assists patients who have a high BMI reach the needed surgery — rather than turning them away — and refers patients for optimization. After patients in this situation meet goals and have surgery, Mayo Clinic offers teams to manage any potential complications.
The choice of how to pursue optimization rests with the patient, in consultation with the surgeon. This may include working with the patient to eliminate smoking, or gain control of diabetes, swelling, ulcers or open wounds — all factors in lowering surgical risk.
Optimization also may include activity modification, injections, medications, and working with bariatric surgery and weight-loss teams to set goals — such as a BMI of 40 or recovering from malnutrition despite the patient's weight — or address any other symptoms. Some patients have bariatric surgery before TKA or THA. In other cases, the surgeon may arrange a weight-loss consult or work with a primary care provider or local weight-loss clinic.
Dr. Bedard is optimistic about potential weight-loss success during optimization. "I've seen many patients who have very high BMI lose weight successfully in the process," says Dr. Bedard.
Dr. Bedard explains that despite optimization, these patients are still at high risk, and the care team must be pragmatic.
"We're unable to eliminate all possible risks," he says. "We're about helping these patients and reducing their surgical risk to a more acceptable level."
Referral considerations for physicians treating patients with high BMI who require arthroplasty
Dr. Bedard indicates multiple options exist for physicians to help patients with a high BMI become ready for a TKA or THA. Community physicians should apply similar pre-surgical optimization strategies as those employed by Mayo Clinic. If a physician does not have access to resources to help optimize patients, one option to consider is referring the patient to Mayo Clinic.
For more information
Refer a patient to Mayo Clinic.