Dec. 22, 2021
In this Q&A, Elizabeth Ann L. Enninga, Ph.D., a reproductive immunologist at Mayo Clinic in Minnesota, discusses COVID-19 and pregnancy. She approaches this topic from the vantage point of immunological challenges for people who develop COVID-19 while carrying a fetus. Dr. Enninga published a systematic review on this topic in a 2020 issue of Mayo Clinic Proceedings. She offers perspectives from time of publication — pre-vaccine — to today, when vaccines are available to the pregnant population.
What pregnancy and COVID-19 data existed before your August 2020 publication?
Virtually none. This was pre-vaccine; we had lots of adult data generally, but not for pregnant women.
What are COVID-19 risks during pregnancy?
Pregnant women are at an increased risk of more-severe severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, including hospitalization and less favorable pregnancy outcomes, such as severe maternal and fetal complications.
Is contracting COVID-19 significant in pregnancy?
Pregnancy, COVID-19 and mechanisms of vascular damage
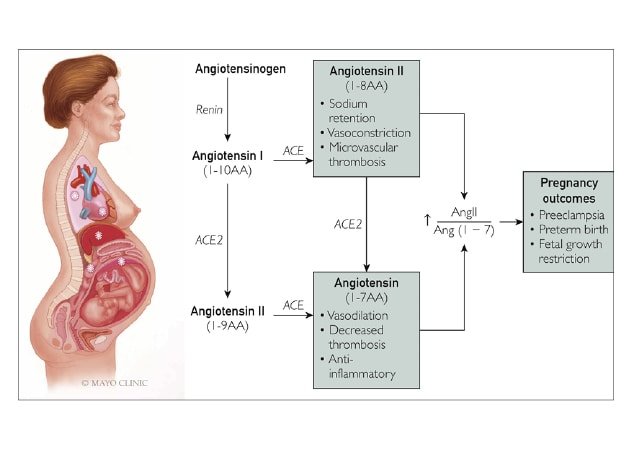
Pregnancy, COVID-19 and mechanisms of vascular damage
Upregulation of angiotensin-converting enzyme 2 (ACE2) receptor in pregnancy may increase the risk of severe acute respiratory syndrome coronavirus 2 infection. Binding of virus to ACE2 causes its downregulation and may increase angiotensin (Ang) II relative to Ang (1-7), thus favoring vasoconstriction, which can mimic or worsen vascular dysfunction in preeclampsia.
It's huge. Severe infection risks are significantly higher in pregnant women compared with same-age nonpregnant women. The mother's respiratory and cardiovascular systems change during pregnancy to support healthy fetal development. Pregnancy affects the renin-angiotensin system, important for regulating blood pressure.
The mother's cardiovascular system is taxed during a typical pregnancy. Additional stress, such as SARS-CoV-2 infection, can increase serious complications, including preeclampsia and gestational diabetes. The immune system also can overreact, causing excessive inflammation while attempting to prevent infection. Thus, pregnant women with COVID-19 are seen in the intensive care unit (ICU) at risk for preterm birth and cesarean delivery due to severe maternal disease.
What is the virus attacking in pregnant women? Can placentas be COVID-19 positive?
The virus attacks many cells, including those in the upper airway, lungs, digestive system, kidneys and blood vessels — all critical to fetal development. Only a small percentage of placentas appear positive for SARS-CoV-2 infection.
As an immunologist who doesn't see patients yet studies immunological responses in pregnancy, how do you perceive COVID-19 vaccine safety?
Everyone has looked into potential danger; no one wants to harm anyone's pregnancy. All data — animal studies and observational studies of pregnant women — demonstrate that the vaccines are safe and effective. We've found zero data indicating that pregnant women would endanger their babies or future fertility with the COVID-19 vaccine. Pregnant women would possibly be endangering their babies by contracting COVID-19, however, if the disease becomes severe.
Obstetricians are concerned about pregnant women with COVID-19: They cannot predict whether mother or fetus will have mild symptoms or severe, life-threatening disease. Unvaccinated individuals exposed to an abundance of virus are more likely to contract and transmit it. It's the same in pregnant women. If they're vaccinated, the virus will have more difficulty becoming established in the body, protecting against severe disease and decreasing contagion.
Another vaccination benefit during pregnancy is that vaccinated pregnant women offers their babies protective antibodies against COVID-19 through the placenta and later through breastfeeding.
Now that vaccines are available, what are U.S. vaccination rates for pregnant women?
Only 31% of pregnant women in the U.S. are vaccinated, according to latest Centers for Disease Control and Prevention data. Many postpone vaccination until after delivery, concerned about potential fetal effects. However, data indicate that pregnant patients with symptomatic COVID-19 have twice the risk of ICU admission and are 70% more likely to die compared with nonpregnant individuals. These are terrifying numbers.
Are mRNA vaccines, such as COVID-19 vaccines, new? How do they work?
mRNA vaccines aren't really new, but they have been used to protect against diseases uncommon in the U.S., including rabies and Ebola. The beauty of mRNA vaccines is that they act like a Snapchat message: The mRNA provides brief instructions to direct immune cells to create a harmless protein — spike protein — prior to rapid mRNA degradation. Immune cells then work to generate this protein, presenting it to other immune cells that recognize it as foreign and destroy it. This process creates protective immunity recalled in any COVID-19 re-exposure. Your immune system is phenomenal at protecting you. But by training it through vaccine, it will better defend against a virus and decrease hospitalization need.
Do the vaccines affect a baby?
COVID-19 vaccines aren't passed directly to the baby, as mRNA is very short-lived. Data support COVID-19 vaccination as a safe, effective way to protect baby and mother, similar to other vaccines administered during pregnancy, such as the flu and the tetanus, diphtheria and pertussis vaccines.
The first few months of life are critical for a baby's immune system. COVID-19 vaccine can give the infant's immune system added protection by transferring protective antibodies generated by the mother's immune system.
What if pregnant women are concerned that COVID-19 vaccines were rushed through the development process?
Vaccine trials themselves weren't rushed — only paperwork. COVID-19 vaccine data are still rigorously tested, just as with other vaccines. A uniqueness in this pandemic was that groups not typically working together — pharmaceutical companies, academic medicine and government — worked cooperatively. I hope this collaboration continues.
Are studies being published that indicate when pregnant women should be vaccinated?
The American College of Obstetricians and Gynecologists recommends that pregnant women get vaccinated as soon as possible, regardless of trimester.
Any other comments on COVID-19 as an immunologist studying pregnancy and issues with this virus?
COVID-19 is a really confusing disease. It doesn't follow clear patterns, seemingly impacting everyone differently. It's hard to predict effects on a given person: Many are asymptomatic; others lie on the couch for three days and still others are on ventilators. An older person with comorbidities and a marathon runner both can be in the ICU because of COVID-19.
COVID-19 has far worse outcomes than influenza. We've had years to figure out influenza's patterns. Contracting COVID-19 leads to more concerning outcomes than flu, including remaining symptomatic long after recovery. In pregnant women with COVID-19, there's higher morbidity and mortality risk, which is especially concerning with current low vaccination rates in this at-risk population.
Features of SARS-CoV-2

Features of SARS-CoV-2
Features and life cycle of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A. Structure of the SARS-CoV-2 viron. B. Viral entry methods and replication of SARS-CoV-2.
While we learn more about this virus daily, COVID-19 is complicated and still upending lives. Because continued infection promotes viral mutations, including the highly transmissible delta strain, the population hasn't reached herd immunity, and many public health strategies now focus on controlling disease burden. Still, vaccination is the best bet for defeating this foe.
For more information
Narang K, et al. SARS-CoV-2 infection and COVID-19 during pregnancy: A multidisciplinary review. Mayo Clinic Proceedings. 2020;95:1750.
COVID-19 vaccines while pregnant or breastfeeding. Centers for Disease Control and Prevention.
COVID-19 vaccines in pregnancy: conversation guide. The American College of Obstetricians and Gynecologists.
Refer a patient to Mayo Clinic.