Dec. 21, 2019
Direct and cell-based delivery of anti-cancer therapy
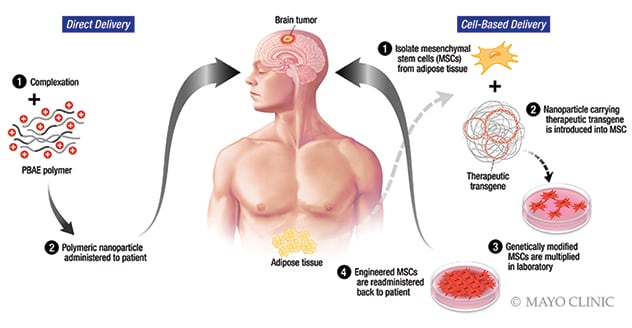
Direct and cell-based delivery of anti-cancer therapy
Mayo Clinic is using nanoparticles for both direct and cell-based delivery of anti-cancer therapy to glioblastomas. The direct delivery method uses a synthetic poly (beta-amino ester) (PBAE) nanoparticle delivery vehicle developed by Mayo Clinic in conjunction with Johns Hopkins University. The cell-based delivery method uses mesenchymal stem cells derived from the patient's adipose tissue.
Mayo Clinic is developing ways to use nanoparticles to deliver anti-cancer therapy directly to glioblastomas. The goal is to devise treatments that effectively target tumor-initiating cells while sparing normal brain cells.
"This technology is extremely promising. We have greater understanding of how these nanoparticles can better penetrate the brain and deliver knockout punches," says Alfredo Quinones-Hinojosa, M.D., chair of Neurosurgery at Mayo Clinic in Jacksonville, Florida, and director of the Brain Tumor Stem Cell Research Laboratory.
Novel therapies for glioblastoma are urgently needed, as life expectancy after diagnosis is 14 to 15 months. Mesenchymal stem cells are an attractive potential drug carrier because they can bypass the blood-brain barrier, travel long distances within the brain, target migrating cancer cells and be modified to deliver anti-cancer agents to tumors.
Viruses, which also are being investigated as potential therapeutic vehicles, pose challenges associated with toxicity and immunogenicity. Nanoparticles are a potential alternative.
"We have observed that cancer cells have a high affinity for the uptake of the nanoparticles we have tested. At the same time, the nanoparticles quickly release their cargo, which improves efficacy," says Hugo Guerrero Cazares, M.D., Ph.D., director of the Neurogenesis and Brain Tumors Laboratory at Mayo Clinic's campus in Florida.
No opportunity wasted
With funding from the National Institutes of Health, Mayo Clinic is studying nanoparticles in vitro and in vivo using laboratory mouse models. One project involves using nanoparticles to modify adipose-derived mesenchymal stem cells to secrete anti-tumor proteins. The nanoparticle-engineered mesenchymal stem cell therapy can be delivered directly into the surgical cavity at the time of tumor resection. "It's a wasted opportunity not to fight the cancer then and there, before we leave the operating room," Dr. Quinones-Hinojosa says.
The project's aims include determining whether nanoparticle-modified stem cells decrease glioblastoma proliferation and invasion in vitro and in vivo. The researchers will also assess the safety and efficacy of treatment with the modified stem cells in combination with targeted radiotherapy in mice with growing patient-derived glioblastomas.
"This technology is becoming much smarter as we develop it," Dr. Quinones-Hinojosa says. "We have learned that these nanoparticles can be loaded with DNA, short interfering RNA and microRNA that will then target the molecular engines that allow cancer cells to migrate. We know the formulation of the most efficient nanoparticles as well as how to make these nanoparticles high throughput and store them for up to three years. Someday, we hope to use these nanoparticles off the shelf in the operating room."
Unlike viruses, Mayo Clinic's novel synthetic nanoparticles can carry many copies of different types of short interfering RNA within single particles. In a study published in the July 2019 issue of Biomaterials, the Mayo Clinic researchers demonstrated that short interfering RNA delivered by the nanoparticles can target several anti-glioblastoma genes simultaneously while avoiding healthy brain cells.
"That opens for us the possibility of combination short interfering RNA therapy, which might be crucial for effective cancer treatment and overcoming tumor resistance," Dr. Guerrero Cazares says. "Glioblastoma is very heterogenous — some part of the tumor might respond to a therapy and others won't. We need to find the right combination of therapies to target all of these tumor pathways."
Exploring new ideas
At Mayo Clinic, research and clinical practice are entwined. With patient consent, tumor tissue is donated to the laboratory for implantation and growth in laboratory mice. Individuals who donate tissue occasionally visit the laboratory; clinicians routinely interact with researchers to advance patient care.
"We work closely with patients and constantly explore new ideas with our surgical department," says Rachel Sarabia Estrada, D.V.M., Ph.D., who assists with directing the Brain Tumor Stem Cell Research Laboratory. "We are very close to moving this technology to the clinic."
"What makes Mayo Clinic thrive is the fact that with every discovery we make, we try to see first and foremost how it can benefit patients," Dr. Quinones-Hinojosa adds. "We can't take care of the needs of the patients unless we translate our discoveries from the lab back to patient care."
For more information
Brain Tumor Stem Cell Research Laboratory. Mayo Clinic.
Kozielski KL, et al. Cancer-selective nanoparticles for combinatorial siRNA delivery to primary human GBM in vitro and in vivo. Biomaterials. 2019;209:79.