Aug. 14, 2020
Mayo Clinic is working to individualize treatment for glioblastoma through advanced imaging and mathematical modeling. A principal focus of these efforts is better use of temozolomide. Although it has been the standard-of-care glioblastoma chemotherapy for more than a decade, the drug's optimal use in individuals hasn't been elucidated.
"The current treatment is homogenized — a standard strategy of six cycles of adjuvant temozolomide for every patient. We believe we might be able to personalize that approach," says Kristin R. Swanson, Ph.D., director of the Mathematical Neuro-Oncology Laboratory at Mayo Clinic in Phoenix/Scottsdale, Arizona.
The laboratory's researchers recently found that temozolomide has a greater effect on nodular tumors than on diffusively invasive tumors, suggesting that patients with less invasive tumors might benefit from additional cycles of the drug. That work builds on the laboratory's earlier discoveries of differences in the molecular mechanisms of glioblastoma tumors in men and women.
"Although we have known that the incidence of glioblastoma is higher in men and that they generally succumb more quickly than women, we haven't known why. This work takes us a step further in personalizing glioblastoma treatment," says Maciej M. Mrugala, M.D., Ph.D., medical director of the Comprehensive Multispecialty Neuro-Oncology Program at Mayo Clinic's campus in Arizona.
Personalized treatments require biomarkers of disease. In the absence of a glioblastoma biomarker, clinicians must rely on MRI. The Mathematical Neuro-Oncology Laboratory seeks to go beyond MRI to provide quantifiable measures of an individual's brain cancer.
"Having a radiomic biomarker of glioblastoma that would allow us to deeply interrogate a tumor — and not just look at it anatomically on the MRI — would be very valuable," Dr. Mrugala says. "Dr. Swanson's models have been able to predict tumor response to various treatments, which brings us closer to that goal."
Quantifying individual tumor behavior
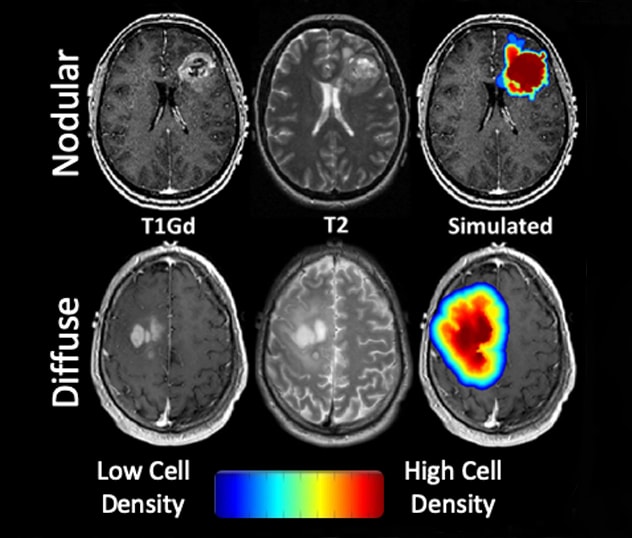
The temozolomide study compared gadolinium-enhanced T1-weighted and T2 fluid-attenuated inversion recovery images taken before and after adjuvant treatment. The images were used to determine volumetric changes in imaging abnormalities and to calculate a tumor invasion metric based on mathematical modeling.
Different extents of tumor invasion beyond the edge seen on MRI
Different extents of tumor invasion beyond the edge seen on MRI
Gadolinium-enhanced T1-weighted and T2 fluid-attenuated inversion recovery images show differing levels of density in glioblastoma tumors. Less color is apparent in the nodular tumor in the top row, while greater color illustrates the higher volume of tumor cells found on biopsy of the diffuse tumor shown in the bottom row.
As described in the March 2020 issue of PLOS One, nodular tumors tended to respond more favorably to adjuvant temozolomide, in terms of both volumetric change and patient outcomes. "The less invasive the tumor looks, the greater the decrease in tumor volume and the longer the patient will have a sustained response to temozolomide," Dr. Swanson says.
She notes that the greater response in nodular tumors might be due to higher concentrations of temozolomide in the tumor core, where the blood-brain barrier is likelier to be compromised compared with surrounding tissue. "In a diffuse glioblastoma, the tumor cells have migrated so far that the blood-brain barrier is still intact in those regions," Dr. Swanson says. "The drug is not going to get there."
Mayo's previous study on sex differences in glioblastoma outcomes — described in the Jan. 2, 2019, issue of Science Translational Medicine — applied a computational algorithm to male and female transcriptome data. In men receiving standard glioblastoma treatment, survival correlated with the expression of cell cycle regulators. In women, survival correlated with the expression of integrin signaling pathway components.
"The biology of the tumor appears to be different in men and women," Dr. Mrugala says. "That might be one reason females have potentially responded better to standard treatment."
Future work might look for sex differences in temozolomide response. "We are finding reasons, based on our imaging and sex differences studies, to think about different strategies for treating glioblastoma," Dr. Swanson says. "Our goal is to use the tools in our arsenal, such as temozolomide, to the best of our ability. That means taking a more personalized approach."
For more information
Massey SC, et al. Image-based metric of invasiveness predicts response to adjuvant temozolomide for primary glioblastoma. PLOS One. 2020;15:e0230492.
Yang W, et al. Sex differences in GBM revealed by analysis of patient imaging, transcriptome, and survival data. Science Translational Medicine. 2019;11:eaao5253.
Mathematical Neuro-Oncology Laboratory: Kristin R. Swanson. Mayo Clinic.