June 28, 2016
Although acoustic neuromas are benign, they can severely affect quality of life. Unilateral hearing loss and tinnitus are common symptoms, and hearing loss can persist after treatment.
Observation might be a valid treatment strategy for small, slow-growing acoustic neuromas; however, patients can experience significant anxiety after a tumor diagnosis. When immediate treatment is indicated, physicians and patients must choose between highly specialized options.
Mayo Clinic in Rochester, Minnesota, has strong experience treating acoustic neuroma with a range of treatment options. Treatment is tailored to the needs, both immediate and long term, of the individual patient.
"Acoustic neuroma is a rare disorder that requires very specialized treatment. We have decades of experience and also have done a great deal of research looking at what patients experience after treatment," says Michael J. Link, M.D., a consultant in Neurosurgery at Mayo Clinic's campus in Minnesota.
Individualized treatment decisions
Acoustic neuromas, which develop in only two to four people per 100,000, are typically discovered on MRI after patients present with unilateral hearing loss, tinnitus, and sometimes dizziness or headache. Surgical removal was once standard treatment; however, reduced tolerance of post-treatment morbidity has resulted in a greater proportion of patients undergoing observation or stereotactic radiosurgery.
In a study published in the September 2015 issue of Otolaryngology — Head and Neck Surgery, Mayo Clinic researchers found that although the incidence of acoustic neuroma has remained steady over time, tumor size at time of diagnosis has decreased. The researchers also noted a clear, recent evolution in the United States toward managing acoustic neuroma with observation.
"Only about 30 percent of acoustic neuromas show growth four years after diagnosis. In the remaining 70 percent of cases, we can just watch for a while," Dr. Link says. "But in those cases, patient anxiety must be managed. A major finding of our research is that having a diagnosis of acoustic neuroma significantly impacts a person's quality of life, even though the tumor is benign and possibly small."
In addition to reassurance, Mayo Clinic patients have follow-up MRI and hearing tests six months after diagnosis, and yearly after that.
Large left acoustic neuroma
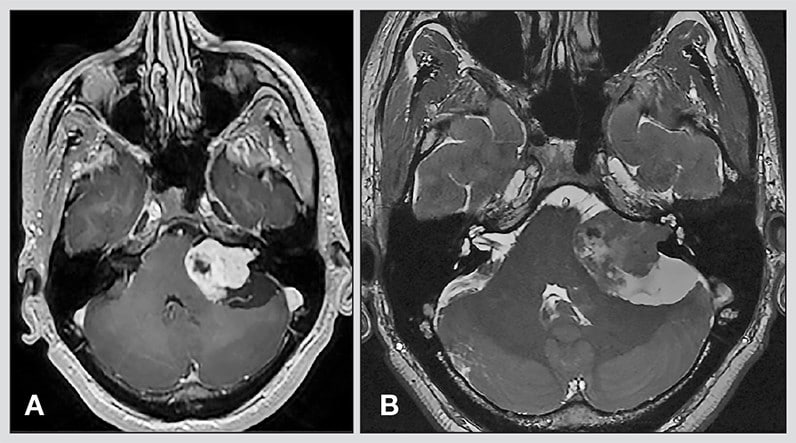
Large left acoustic neuroma
A. Preoperative axial T1 post-gadolinium imaging reveals a large left acoustic neuroma. B. Postoperative imaging three months after removal of the tumor shows complete resection.
Treatment is generally recommended for patients whose tumors are growing or who have symptoms amenable to treatment, particularly if those patients are young. Outcomes are generally good, whether treatment involves stereotactic radiosurgery or surgical removal of the acoustic neuroma.
"When treated by an experienced team, most patients with small to medium tumors experience high rates of tumor control and excellent facial nerve outcomes, regardless of treatment modality," Dr. Link says. Indeed, in the largest quality-of-life study conducted among patients with acoustic neuromas, published in the April 2015 issue of the Journal of Neurosurgery, Mayo Clinic researchers and colleagues in Bergen, Norway, found that patient-related factors such as overall physical and emotional health have a stronger impact on quality of life than treatment strategy does.
Although tumors can be successfully controlled, many patients continue to experience symptoms after treatment. Regardless of treatment strategy, the long-term prospects for hearing in the affected ear are poor. More than 75 percent of patients studied had nonserviceable hearing in the affected ear eight years after treatment for acoustic neuroma, according to a paper by the Mayo Clinic and Bergen researchers published in the August 2015 issue of Neurosurgery.
Similarly, as described in a study published in the November 2015 issue of the Journal of Neurosurgery, long-term severe headache is driven more by patient-related factors than by tumor size or treatment modality. Treatment modality also doesn't appear to affect long-term dizziness, as described in a Mayo Clinic study in the December 2014 issue of Otolaryngology — Head and Neck Surgery.
"We've learned that there's not a big advantage of one treatment over another for long-term quality of life," Dr. Link says. "But when we spend time talking with a patient, we can usually figure out the best treatment for that individual. If a patient says, 'I can't live like this; I have to get this tumor removed,' then we can tell the patient what we think life will be like eight years from now if the tumor is removed using surgery, or if the patient receives stereotactic radiosurgery and the tumor is controlled."
Expertise with radiation and surgery
Mayo Clinic was among the first centers in the United States to offer Gamma Knife radiosurgery. Over the past 26 years, it has been used at Mayo Clinic's campus in Minnesota to treat approximately 1,000 acoustic neuromas. In addition, Mayo Clinic neurosurgeons have surgically removed thousands of acoustic neuromas.
Otolaryngologists work with neurosurgeons on each case. Intraoperative monitoring is used to avoid damaging auditory, facial and other cranial nerves. "We think it's important to take out all of the tumor. But sometimes we do a less than complete resection to keep the facial nerve intact," Dr. Link says. "We follow up on those patients and might treat them with Gamma Knife radiation down the road, if the tumor grows."
Patients who continue to experience severe headache after treatment can be referred to Mayo Clinic neurologists who specialize in headache. Vestibular rehabilitation is offered to patients with balance problems.
"All of the treatment strategies for acoustic neuroma have advantages and disadvantages," Dr. Link says. "We are starting to learn that if a tumor is fast-growing, it might not respond as well to radiation. In those cases we tend to lean toward surgery. But we look at each case individually to determine what is best for that patient."
For more information
Carlson ML, et al. The changing landscape of vestibular schwannoma management in the United States — A shift toward conservatism. Otolaryngology — Head and Neck Surgery. 2015;153:440.
Carlson ML, et al. Long-term quality of life in patients with vestibular schwannoma: An international multicenter cross-sectional study comparing microsurgery, stereotactic radiosurgery, observation, and nontumor controls. Journal of Neurosurgery. 2015;122:833.
Tveiten OV, et al. Long-term auditory symptoms in patients with sporadic vestibular schwannoma: An international cross-sectional study. Neurosurgery. 2015;77:218.
Carlson ML, et al. Risk factors and analysis of long-term headache in sporadic vestibular schwannoma: A multicenter cross-sectional study. Journal of Neurosurgery. 2015;123:1276.
Carlson ML, et al. Long-term dizziness handicap in patients with vestibular schwannoma: A multicenter cross-sectional study. Otolaryngology — Head and Neck Surgery. 2014;151:1028.