April 13, 2019
Acute pancreatitis (AP) is the most common hospital gastroenterology discharge diagnosis. This condition is characterized by sudden and severe abdominal pain and elevated levels of pancreatic enzymes. In cases that involve necrosis of either the pancreas or the peripancreatic fat, AP carries a risk of substantial morbidity and mortality.
AP has multiple etiologies, with cholelithiasis and alcohol abuse accounting for the majority of cases. Less common causes include hypertriglyceridemia, use of certain medications and pancreatic duct injury. And in rare cases, biliary sludge, biliary obstruction, hypercalcemia, infections and toxins, vascular diseases, and anatomic anomalies can also be a cause. Up to 30 percent of patients have idiopathic AP, with no identifiable etiology.
Each of these etiologies can trigger the activation of multiple parallel signaling pathways in pancreatic cells that can cause cell injury or inflammation. The fact that AP can progress by using these parallel signaling pathways can reduce the efficacy of targeted pharmacotherapy. To address this challenge, a team of researchers studied whether inducing hypothermia in the pancreata of rats could reduce the severity of AP induced by different methods.
Research methods
Researchers inserted a urethane balloon with two polyurethane tubes inside the stomach of Wistar rats. They induced AP by administering the mechanistically distinct agents cerulein or glyceryl tri-linoleate (GTL). Rats in the treatment group received infused cold water in the balloon to cool the pancreas to temperatures found to decrease acinar cell injury. Rats in the control group received an unperfused balloon.
The research team monitored pancreatic and rectal temperatures and prevented generalized hypothermia using an infrared lamp or heating pad. Researchers studied the uptake of a 2-deoxyglucose tracer, and they collected and analyzed blood, pancreas, kidney and lung tissues using histology, immunofluorescence, immunoblot, cytokine and chemokine magnetic bead, and DNA damage assays. By documenting any injury to acinar cells, they gauged the effect of hypothermia on signaling pathways initiated by cerulein and GTL.
Research findings
The researchers shared a number of findings from this study in an article published in Gastroenterology. According Vijay P. Singh, M.B.B.S., the article's lead author, the study yielded findings that they hope will improve the understanding of how best to manage this condition. Dr. Singh is a gastroenterologist at Mayo Clinic's campus in Arizona whose research focuses on the pathophysiology of acute and chronic pancreatitis.
Mild and severe acute pancreatitis
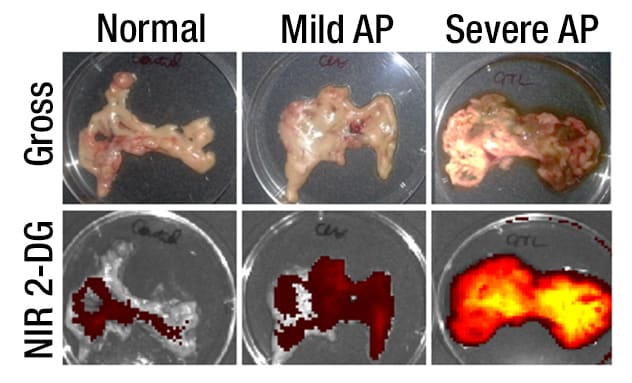
Mild and severe acute pancreatitis
Pancreata show gross appearance and uptake of near infrared 2-deoxyglucose (NIR 2-DG) in mild and severe acute pancreatitis.
"We established that local pancreatic hypothermia can be induced transgastrically and used therapeutically to slow multiple signaling cascades simultaneously in pancreatitis," explains Dr. Singh. "And we demonstrated the ability of a minimally toxic, rapidly inducible and reversible treatment to reduce local and systemic injury associated with both mild and severe pancreatitis, irrespective of this condition's diverse etiologies."
Early transgastric pancreatic cooling
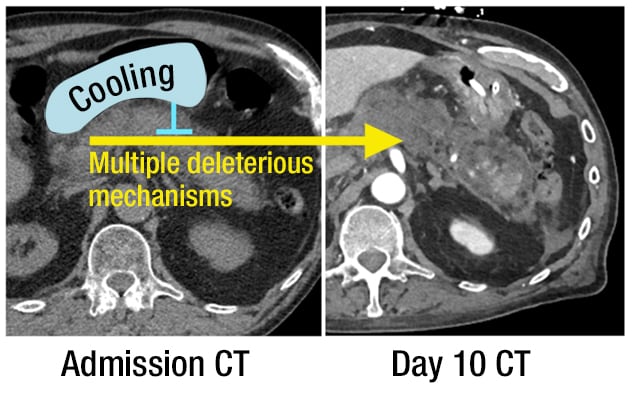
Early transgastric pancreatic cooling
Proposed role of early transgastric pancreatic cooling uses the balloon (blue) in preventing the progression of acute pancreatitis to a severe disease.
Significant findings include the following:
- Rats in the treatment group developed less severe GTL-induced AP compared with rats in the control group.
- In acinar cells, cooling decreased the lipolysis induced by GTL, increased the micellar form of its fatty acid, reduced the increase in cytosolic calcium, prevented the loss of mitochondrial membrane potential (by 70 to 80 percent), and resulted in a 40 to 50 percent decrease in the uptake of a fatty acid tracer.
- Rats in the treatment group had decreased pancreatic necrosis, decreased serum levels of cytokines and markers of cell damage, and decreased markers of lung and renal damage.
- Pancreatic cooling increased the proportion of rats surviving six hours after induction of AP (90 percent in the treatment group, versus less than 10 percent in the control group).
- Rats with severe, GTL-induced AP had earlier and higher pancreatic uptake of the 2-deoxyglucose tracer than did rats with milder, cerulein-induced AP.
- Rats in the treatment group with cerulein-induced AP had decreased pancreatic markers of apoptosis and inflammation.
Conclusions and next steps
This study demonstrated that transgastric local pancreatic hypothermia decreases pancreatic necrosis, apoptosis, inflammation and markers of pancreatitis severity and increases survival in an animal model.
"We are hopeful that this animal study will provide the basis for novel, translatable, scientifically sound methods of predicting severe AP and reducing its severity, irrespective of its etiology," says Dr. Singh. "The rapid, multimodal effect of cooling could be employed as an early intervention to prevent clinical worsening over the first several hours or days until an approach tailored to the specific etiology (such as plasmapheresis or stone extraction) can be administered, or until the offending toxin (such as alcohol) is metabolized or excreted."
For more information
De Olivera C, et al. Multimodal transgastric local pancreatic hypothermia reduces severity of acute pancreatitis in rats and increases survival. Gastroenterology. 2019;156:735.