Feb. 12, 2022
In many animals, the digestive process takes hours and occurs within the tightly sealed GI tract. As researchers attempt to better understand digestion in humans, they have hypothesized that the GI tract, much like the skin and oral cavity, must be equipped with specialized sensory capabilities that allow it to assess the chemical and physical properties of the luminal contents.
Mayo Clinic gastroenterologist and researcher Arthur Beyder, M.D., Ph.D., and colleagues believe that the GI epithelium contains specialized sensory enteroendocrine cells (EECs) that interact with the luminal contents and function as sensors of luminal nutrients, microbial metabolites and mechanical forces. Dr. Beyder's laboratory is located at Mayo Clinic's campus in Rochester, Minnesota.
Gut touch sensors in mouse small bowel
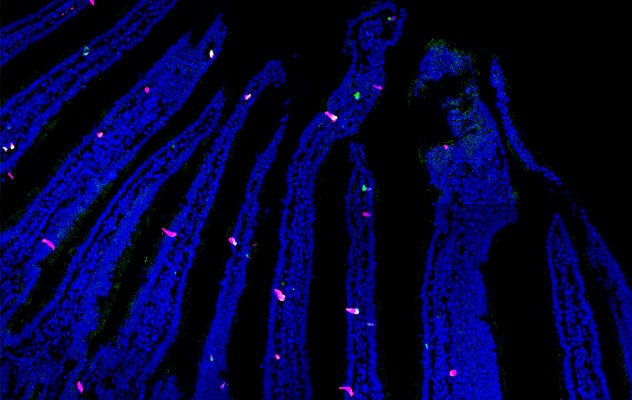
Gut touch sensors in mouse small bowel
Fluorescence image shows sporadically distributed gut touch receptors (magenta), which make up less than 1% of all epithelial cells (blue) in mouse small bowel.
Super resolution image of a single gut touch sensor

Super resolution image of a single gut touch sensor
Super resolution microscopy shows a typical gut touch sensor with Piezo2 mechanosensors (yellow), packed with serotonin (magenta) and nucleus (blue), and surrounded by actin (cyan), which serves as important structural element. Based on Proceedings of the National Academy of Sciences. 2018;115:E7632.
Optogenetic gut touch sensors

Optogenetic gut touch sensors
Fluorescence image shows optogenetic gut touch receptors (green) surrounded by epithelial cells (blue) in mouse colon.
Optogenetic gut touch cell
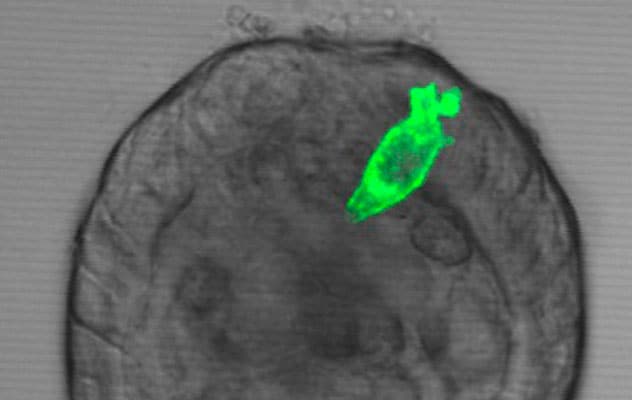
Optogenetic gut touch cell
Light and fluorescence image shows an optogenetic gut touch cell in an organoid with the mini-gut lumen inside and the gut touch receptor positioned optimally to sense the physical properties of luminal contents in a process called gut touch. Based on Gastroenterology.
EECs are thought to be similar to specialized epithelial cells within the oral cavity and skin that contribute to the sensations of taste and touch. One type of EEC in the GI tract expresses a mechanically gated ion channel called Piezo2 that is also found in the skin's Merkel cells, which contribute to the sensation of touch. Building on this understanding, Dr. Beyder and co-investigators sought to further examine the role of Piezo2+ EECs and to determine whether these cells endow the gut with some form of tactile sensitivity. These Piezo2+ EECs are known as "gut touch sensors."
"Our study explores the concept of gut touch — that the gut can 'touch' and 'feel' what's inside and modify its function based on physical properties of what's in the lumen — which is important because many treatments for our patients involve modifications of the physical properties of their diets," says Dr. Beyder.
The researchers used a range of established and novel techniques, in single cells and living animals. These techniques included single-cell RNA sequencing and opto-electrophysiology, opto-organ baths with luminal shear forces, and in vivo studies that assayed GI transit while manipulating physical properties of luminal contents. The results of these studies were published in Gastroenterology in 2022.
Results and conclusions
Dr. Beyder and co-authors reported a number of significant findings and observations, including the following:
- Gut touch sensors may be synaptically connected to epithelial sensory cells.
- Activation of gut touch sensors by light or forces led to Piezo2-dependent alterations in colonic contractions driven by intrinsic circuitry.
- When gut touch sensors were eliminated, mouse small bowel and colon lost the capability to detect small luminal forces and luminal contents' physical properties to regulate transit times in the small and large bowel.
"Our findings suggest that the gut touch sensors that release serotonin in response to small forces regulate important aspects of digestion. This system may be similar to the mechanical sensors in the skin and oral cavity that sense touch and food texture," says Dr. Beyder. "Gut touch sensors allow the GI tract to detect luminal forces and physical properties of luminal contents to modulate physiology."
Potential clinical implications
Dr. Beyder's team is excited to move this work forward. He explains that these study results in mouse models may have multiple potential implications for clinical practice in the future.
"By gaining a better understanding of how GI epithelial mechanosensitivity mediates gut touch, which contributes to the regulation of GI motility, we may be able to apply this knowledge to how we treat GI functional and motility disorders. We can now explore whether this newly discovered sensory process exists in humans and if it is affected in diseases such as IBS and, potentially, in patients who have overlapping neurological sensory and gastrointestinal sensation and motility abnormalities."
According to Dr. Beyder, this new knowledge may shed light on how and when dietary modifications are appropriate for managing some diagnoses. "We know that modification of dietary components in a large proportion of our patients improves symptoms. However, we still do not understand how these modified diets work."
Dr. Beyder and colleagues continue to perform research that explores and further develops this paradigm and its possible applications to treating patients with gastrointestinal disorders. "A great deal more research is needed to fully understand the gut touch sensory process," he explains. "We discovered the receptors but need to define the sensory circuit, understand the mechanisms of touch sensing, and explore this in healthy humans and in humans with disease."
For more information
Treichel AJ, et al. Specialized mechanosensory epithelial cells in mouse gut intrinsic tactile sensitivity. Gastroenterology. 2022;162:535.
Refer a patient to Mayo Clinic.