Diagnosis
To diagnose cholecystitis, your healthcare professional does a physical exam and asks about your symptoms and medical history. Tests and procedures used to diagnose cholecystitis include:
- Blood tests. Blood tests can look for signs of an infection or other gallbladder issues.
- Imaging tests that show your gallbladder. Abdominal ultrasound, endoscopic ultrasound, CT scan or magnetic resonance cholangiopancreatography can make pictures of your gallbladder and bile ducts. These pictures may show signs of cholecystitis or stones in the bile ducts and gallbladder.
- A scan that shows the movement of bile through the body. A hepatobiliary iminodiacetic acid (HIDA) scan tracks the making and flow of bile from the liver to the small intestine. A HIDA scan involves putting a radioactive dye into your body. The dye attaches to the cells that make bile. During the scan, the dye can be seen as it travels with the bile through the bile ducts. This can show any blockages.
Treatment
Endoscopic retrograde cholangiopancreatography
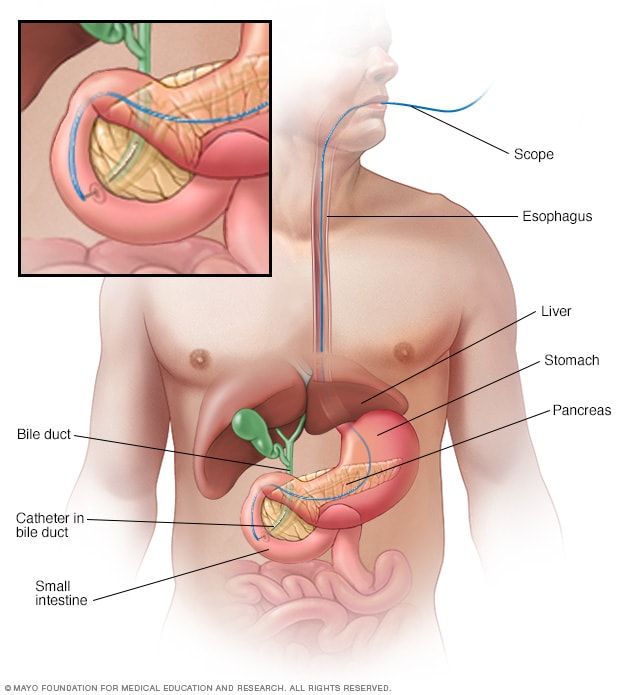
Endoscopic retrograde cholangiopancreatography
Endoscopic retrograde cholangiopancreatography (ERCP) uses a dye to highlight the bile ducts on X-ray images. A thin, flexible tube with a camera on the end, called an endoscope, goes through the throat and into the small intestine. The dye enters the ducts through a small hollow tube, called a catheter, passed through the endoscope. Tiny tools passed through the catheter also can be used to remove gallstones.
Laparoscopic cholecystectomy
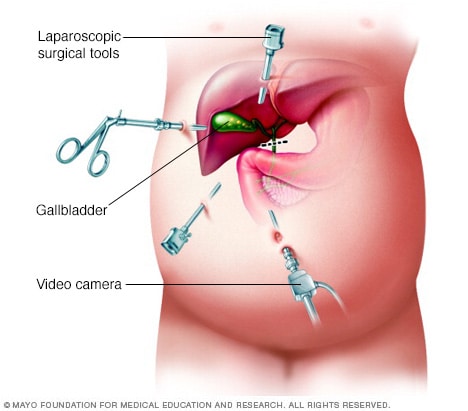
Laparoscopic cholecystectomy
Special surgical tools and a tiny video camera are put through cuts, called incisions, in the belly during laparoscopic cholecystectomy. Carbon dioxide gas inflates the belly to make room for the surgeon to work with surgical tools.
Treatment for cholecystitis most often involves a hospital stay to control the swelling and irritation, called inflammation, in your gallbladder. Sometimes, surgery is needed.
At the hospital, treatments to control your symptoms may include:
- Fasting. You may not be able to eat or drink at first to take stress off your inflamed gallbladder.
- Fluids through a vein in your arm. This treatment helps prevent loss of body fluids, called dehydration.
- Antibiotics to fight infection. You might need these if your gallbladder is infected.
- Pain medicines. These can help control pain until the inflammation in your gallbladder is relieved.
- Procedure to remove stones. You may have a procedure called an endoscopic retrograde cholangiopancreatography (ERCP). This procedure uses dye to make the bile ducts show up during imaging. Then a healthcare professional can use instruments to remove stones blocking the bile ducts or cystic duct.
- Gallbladder drainage. Sometimes, gallbladder drainage, called cholecystostomy, can remove infection. You might have this procedure if you can't have surgery to remove your gallbladder. To drain the gallbladder, a healthcare professional can go through the skin on the belly. This method is called percutaneous drainage. Or the health professional could pass a scope through the mouth, called endoscopic drainage.
Your symptoms are likely to get better in 2 to 3 days. But gallbladder inflammation often returns. In time, most people with cholecystitis need surgery to remove the gallbladder.
Gallbladder removal surgery
The procedure to remove the gallbladder is called a cholecystectomy. Most often, this is a minimally invasive procedure called laparoscopic cholecystectomy. This type of surgery uses a few tiny cuts called incisions in your belly. An open procedure, in which a long incision is made in your belly, is rarely needed.
The timing of surgery depends on how bad your symptoms are and your overall risk of complications during and after surgery. If your surgical risk is low, you might have surgery during your hospital stay.
Once your gallbladder is removed, bile flows from your liver into your small intestine, rather than being stored in your gallbladder. You can still digest food without a gallbladder.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Preparing for your appointment
Make an appointment with your healthcare professional if you have symptoms that worry you. For cholecystitis, you may be sent to a specialist in the digestive system, called a gastroenterologist. Or you may be sent to a hospital.
What you can do
Before your appointment:
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet.
- Make a list of your symptoms, including any that don't seem related to the reason for your appointment.
- Make a list of key personal information, including major stresses or recent life changes.
- Make a list of all medicines, vitamins, herbs and other supplements that you take, including doses.
- Take a family member or friend along, if possible. Someone who goes with you can help you gather information you get.
- Make a list of questions to ask your healthcare professional.
For cholecystitis, some basic questions to ask include:
- Is cholecystitis the likely cause of my belly pain?
- What are other possible causes for my symptoms?
- What tests do I need?
- Do I need to have my gallbladder taken out?
- How soon do I need surgery?
- What are the risks of surgery?
- How long does it take to recover from gallbladder surgery?
- Are there other treatments for cholecystitis?
- Should I see a specialist?
- Are there brochures or other printed material that I can take with me? What websites do you suggest?
Be sure to ask all the questions you have.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including:
- When did your symptoms begin?
- Have you had pain like this before?
- Are your symptoms constant or do they come and go?
- How bad are your symptoms?
- What, if anything, seems to make your symptoms better?
- What, if anything, seems to make your symptoms worse?
Oct. 23, 2024