Dec. 29, 2018
Mayo Clinic uses a novel modification of the superior capsule reconstruction (SCR) technique for enhanced treatment of massive irreparable rotator cuff injuries. Early results of the surgical technique, offered to patients with Hamada grade 2 and 3 tears, are promising.
"We use an acellular human dermal allograft to perform an SCR. But we use the leftover allograft to resurface the undersurface of the acromion, which effectively doubles the thickness of the construct and may provide more-durable outcomes, especially for younger and more-active patients," says John M. Tokish, M.D., an orthopedic surgeon at Mayo Clinic in Phoenix, Arizona.
Reverse shoulder arthroplasty can restore function and improve pain in older patients with severe rotator cuff injuries. But patients under age 65 may experience increased complications from the procedure compared with older patients.
"With this SCR-plus technique, we've been able to reconstruct the acromiohumeral interval. When we add biologics such as platelet-rich plasma into the graft, we can increase the healing rate and can provide an alternative to arthroplasty," Dr. Tokish says.
Thickness similar to autograft
The original SCR technique used a fascia lata autograft, which was folded two or three times to obtain a graft thickness of 6 to 8 millimeters (mm). Clinical outcomes of these procedures were comparable to outcomes of complete rotator cuff repairs. But donor site morbidity associated with autograft led to the use of dermal allografts in SCR, which has been less successful.
"The maximum thickness of commercially available dermal allografts is about 3.5 mm — half that of the autografts used in the original SCR technique and below the thickness of the native capsule," Dr. Tokish says.
Dermal allografts are significantly more expensive than autografts, making it financially unfeasible to use a second graft to achieve the desired thickness. "But the allografts are usually large enough to provide two separate grafts," Dr. Tokish says.
Parches de aloinjerto dérmico humano en su lugar
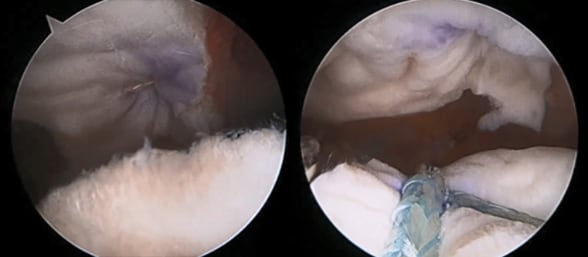
Parches de aloinjerto dérmico humano en su lugar
Las fotografías muestran los parches de aloinjerto dérmico humano en su lugar después del procedimiento modificado de Mayo Clinic para la reconstrucción de la cápsula superior. A la izquierda, el primer aloinjerto se encuentra en la posición típica para este procedimiento. A la derecha, un segundo aloinjerto se coloca en el acromion.
The first allograft is attached to the glenoid and greater tuberosity, as is typically done in SCR, and the second to the underside of the acromion. The grafts are positioned with the epidermal sides opposed, to create a healing layer between the graft and the humeral head, and between the graft and the bare bone of the acromion. "There's a healing and a gliding surface on both grafts, as well as 8 mm of graft thickness in the subacromial space," Dr. Tokish says.
Recovery takes about six months, to allow the grafts to become incorporated. Mayo Clinic provides a physical therapy regimen for restoration of motion and strengthening of the joint. "The ideal candidate for this SCR-plus procedure would be a younger active patient with a failed rotator cuff repair or a new large-to-massive rotator cuff injury," Dr. Tokish says.
"Rotator cuff injuries are common, and they keep people from doing what they love to do," he adds. "SCR-plus is a next step in our evolving efforts to manage these injuries, but I don't think it's the final step. We are becoming much more attuned to the benefits of biologics. That partnership between individualized medicine and surgery will help us find solutions to the injuries, and we're in hot pursuit."