Feb. 09, 2022
Mayo Clinic has launched a multidisciplinary effort to reduce the risk of postoperative infections in patients with underlying conditions who have hip or knee replacements. The most common underlying conditions that increase that risk are obesity and diabetes.
"These infections are devastating. We are committed to decreasing the risk factors for poor prognosis in this subset of patients," says Rafael J. Sierra, M.D., chair of Adult Reconstruction, Orthopedic Surgery, at Mayo Clinic in Rochester, Minnesota. "The goal is for the patient ultimately to get the hip or knee replacement. But first we want to work on the comorbidities, to optimize surgical outcomes."
Patients who are identified as being at high risk — and who agree to work on their risk factors before having joint replacement surgery — are referred to Mayo Clinic's Endocrinology, Diabetes, Metabolism, and Nutrition, one of the largest divisions of its kind in the world.
"We work with these patients not only to optimize their weight management and diabetes care but also to help them develop new goals and regain function," says Juan P. Brito Campana, M.B.B.S., an endocrinologist at Mayo Clinic's campus in Minnesota. "In addition to addressing biomedical issues, we address the wider context of these individuals' lives."
The approach requires balancing individuals' desire for joint replacements that can ultimately relieve pain with surgeons' desire to maximize outcomes. "In the past, we've seen a lack of communication about what patients want and what surgeons want," Dr. Sierra says. "But respectful conversations with patients can help them set goals and help us better prepare them for orthopedic surgery."
Patient-centered, respectful approach
Mayo Clinic appointment coordinators screen individuals referred for joint replacement to identify potential risk factors. Specific questions involve height and weight, use of tobacco and narcotics, and level of diabetes control if that condition is present. Individuals identified as being at high risk are contacted by a specially trained orthopedic nurse, who explains the approach for reducing risk.
"The nurse follows a script that has been vetted by our orthopedic and endocrinology groups. There are specific words that can and cannot be used," Dr. Sierra says. Patients who wish to learn more have a virtual meeting with an endocrinology nurse who forwards information about the risk-reduction program. Individuals can then decide whether to join.
"Some patients are happy to have this focus on risk reduction. For others, it's a hard sell," Dr. Sierra says. "Many patients have been denied a joint replacement elsewhere because of their risk factors and have come to Mayo Clinic as a last resort."
Riesgo relativo de infección profunda
Riesgo relativo de infección profunda
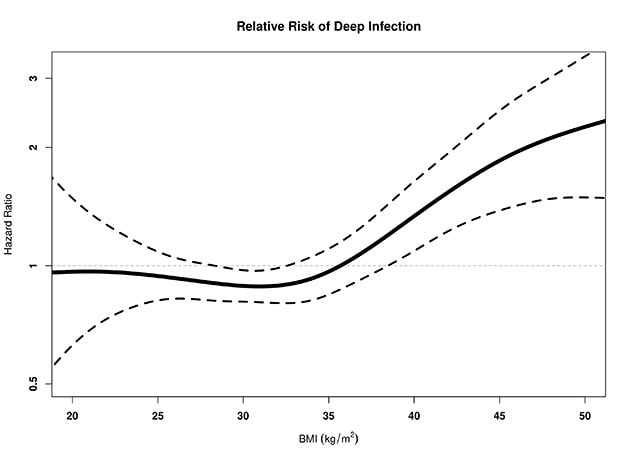
La línea continua del gráfico muestra el índice de riesgo de infección profunda en función del índice de masa corporal tras la artroplastia total de rodilla. Las líneas negras punteadas indican el intervalo de confianza del 95 %. La línea gris punteada indica dónde estaría la línea si no hubiera mayor o menor riesgo de infección.
The risk of infection after joint surgery for people with a body mass index (BMI) above 40 or 50 is as much as triple the risk for people with lower BMI. "Sometimes patients tell us they'll take that risk," Dr. Sierra says. "They don't understand that if they get an infection, they might face more surgery or even potentially amputation. That's why education is very important."
Individuals who join the risk-reduction program see specialists in Mayo Clinic's advanced weight management program and the Diabetes Mellitus Specialty Group, part of Mayo's highly ranked endocrinology division.
"We have a multidisciplinary team of endocrinologists, dietitians, psychiatrists, and physical medicine and rehabilitation specialists to help patients in this transition to orthopedic surgery care," Dr. Brito Campana says. "These patients have pain and difficulty moving around and might have issues with getting or maintaining a job. We work with them to optimize their weight management and diabetes care — and at the same time to maximize the overall functioning of their lives."
Once patients achieve their goals, Orthopedic Surgery schedules their joint replacements. The process is individualized to each patient.
"We can't have the same goals for everyone," Dr. Sierra says. "Helping a person lower BMI from 60 to 45 is a big deal. For a person who starts at a BMI of 40, getting down to 30 makes a difference."
As a fully integrated center of excellence, Mayo Clinic can provide multispecialty expertise for challenging issues. "We see patients at high risk who had hip or knee replacements elsewhere and were referred to us because of complications," Dr. Sierra says. "Once the complications occur, we are limited in what we can do. We'd rather do the primary hip or knee replacement here once we have worked to optimize outcomes."
For more information
Refer a patient to Mayo Clinic.