Oct. 01, 2021
Diabetic retinopathy is the leading cause of preventable blindness among working-aged adults. It affects more than 33% of patients with diabetes mellitus. Among these patients, diabetic macular edema (DME) remains a leading cause of visual impairment. "Patients with diabetes mellitus are also more likely to develop cataracts and tend to develop them at a younger age compared with other patients. When patients with DME develop visually significant cataracts, a relevant question is whether cataract surgery will worsen the diabetic eye disease," says Sophie J. Bakri, M.D., chair of Ophthalmology at Mayo Clinic in Rochester, Minnesota.
To investigate that question, Dr. Bakri and fellow researchers performed a retrospective chart review of all patients with active DME who received treatment with intravitreal anti-vascular endothelial growth factor (anti-VEGF) injections before and after cataract surgery at Mayo Clinic in Rochester, Minnesota, from Jan. 1, 2012, through Dec. 31, 2017. The use of intravitreal anti-VEGF agents is an established treatment for DME.
Edema macular diabético que afecta al centro
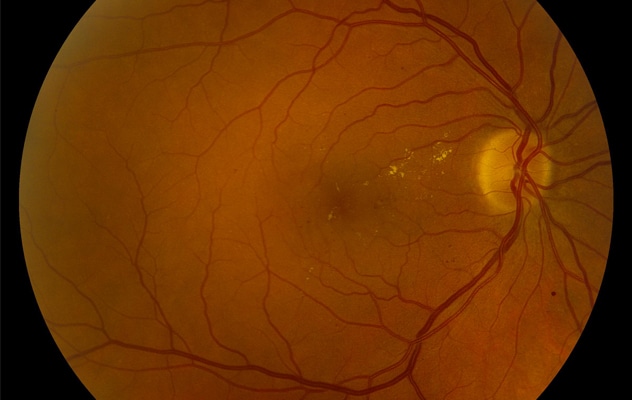
Edema macular diabético que afecta al centro
Los criterios de inclusión del estudio incluyeron el diagnóstico del edema macular diabético en el ojo operativo.
Inclusion criteria included diagnosis of DME in the operative eye and an intravitreal anti-VEGF injection in the operative eye within the six months prior to surgery. In 32 patients with active DME, 40 eyes were actively being managed with ipsilateral intravitreal anti-VEGF injections and were treated with cataract surgery during the five-year study period; 37 eyes of 30 patients were included in the study.
Outcome measures included the development of subretinal or intraretinal fluid in the six months following surgery, timing and number of injections, best corrected visual acuity, and central subfield thickness (CST) on optical coherence tomography (OCT).
"Patients were typically managed with an initial series of 2 to 4 injections at a defined interval (typically every four weeks) and were reevaluated with repeat OCT imaging after the completion of the initial series," notes Dr. Bakri. "Based on the imaging findings and clinical exam, the interval between injections was increased (improved fluid findings on OCT), remained unchanged (stable OCT findings) or was decreased if greater than four weeks (with new fluid findings on OCT)."
Worsening DME does not affect visual acuity
The researchers found a significant improvement between pre- and postoperative best corrected visual acuity when comparing all eyes (P < 0.0001) and no significant difference in CST before and after surgery (P > 0.05). Preoperative OCT found fluid in 30 eyes (81.1%).
Dr. Bakri notes: "Following surgery there was a statistically significant improvement in mean visual acuity without a statistically significant increase in retinal thickness; however, nearly 50% of eyes had some worsening of DME following surgery (although not statistically significant). The increased DME did not appear to affect visual outcomes, and eyes with worse DME still had a significant improvement in visual acuity. There was also no increase in the number of anti-VEGF injections postoperatively.
"Despite the active DME, cataract surgery in the eyes in our study was still successful, with improvement in vision and stable CST measurements. The success is likely owed to the active management with pre- and postoperative anti-VEGF therapy. Therefore, patients with active DME and visually significant cataract can consider cataract surgery while maintaining an effective perioperative intravitreal anti-VEGF regimen when needed — but those patients need to understand that the DME may worsen and perhaps need increased treatment."
Study results were published in the American Journal of Ophthalmology in 2021.
For more information
Starr MR, et al. Outcomes of patients with active diabetic macular edema at the time of cataract surgery managed with intravitreal anti-VEGF injections: Outcomes of cataract surgery in active DME patients. American Journal of Ophthalmology. 2021;229:194.