Aug. 17, 2018
Intraocular lens technology has revolutionized cataract surgery. Cataract surgery is the most common intraocular surgery performed today; it provides dramatic improvement in quality of life and vision. Most patients undergoing cataract surgery do so without significant complications. Some patients, however, require secondary procedures such as intraocular lens exchange, which may be indicated when complications occur related to the primary cataract surgery, or after surgery related to the lens implant or pre-existing disease or trauma.
Most published reports of intraocular lens exchange outcomes originate from tertiary referral centers, preventing a true estimate of the incidence of this procedure in the general population. To identify a population-based incidence rate for pseudophakic intraocular lens exchange, Erick D. Bothun, M.D., Sanjay V. Patel, M.D., and a research team with Ophthalmology at Mayo Clinic's campuses in Rochester, Minnesota, and Jacksonville, Florida, conducted a Rochester Epidemiology Project-based, retrospective study to determine the population-based incidence of pseudophakic intraocular lens exchange in Olmsted County, Minnesota. "The 148,201-member population of Olmsted County, Minnesota, as documented in the Rochester Epidemiology Project, allows a virtually complete ascertainment of all clinically recognized cases of intraocular lens exchange among county residents," says Dr. Bothun.
The research team identified all patients who received intraocular lens exchanges between Jan. 1, 1986, and Dec. 31, 2016. Initial criteria included surgical codes for intraocular lens exchange, secondary intraocular lens implantation and intraocular lens explantation. Intraocular lenses that were exchanged at the primary cataract surgery were not included.
All medical records were reviewed to determine patient demographics, the indication for intraocular lens exchange, the types and locations of the lenses removed and replaced, and the clinical outcomes with length of follow-up.
Caso de disinserción espontánea del háptico de la lente que conduce a la dislocación de la lente
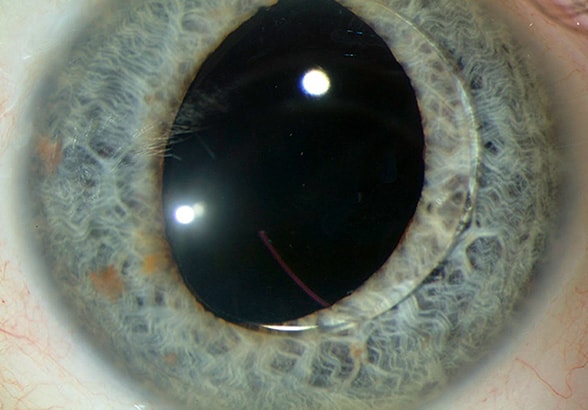
Caso de disinserción espontánea del háptico de la lente que conduce a la dislocación de la lente
Un paciente masculino de 73 años presentó una desinserción espontánea del háptico de una lente endocapsular colocada 16 años antes y 11 años después de una capsulotomía posterior con láser de neodimio: itrio-aluminio-granate que provocó la dislocación de la lente. La lente dislocada fue cambiada por una lente en el surco con soporte capsular. Imagen reimpresa con permiso de la American Journal of Ophthalmology (Revista Estadounidense de Oftalmología).
The indications for intraocular lens exchange were categorized according to pre-defined criteria: Dislocated lenses were those that had sufficiently moved to impair vision (reduced visual acuity, monocular diplopia or glare) or to create complications within the eye. This indication was further categorized as dislocations occurring from capsular tears, zonular weakness, external head or facial trauma, and haptic disinsertion. Subcategories included dislocated lenses causing corneal edema or a uveitis-glaucoma-hyphema syndrome. Other major categories for intraocular lens exchange were corneal edema without lens dislocation, unplanned refractive outcome, optic failure and dysphotopsia.
Changes to incidence and indication
The research team identified 80 people who received intraocular lens exchange, yielding an overall age- and sex-adjusted incidence rate of 28.4 per million (confidence interval, or CI, 22.1 to 34.7), which increased over the study period (P = 0.04). The 30-year cumulative probability of intraocular lens exchange among patients receiving cataract surgery was 1.5 percent (CI, 0.6 to 2.4 percent), and increased at a relatively constant rate.
The majority (72.5 percent) of intraocular lens exchanges were performed for dislocated lenses. More than half of these exchanges were associated with capsular tears that occurred at the primary cataract surgery, or from zonular weakness or corneal edema. Two new indications emerged in the final decade of this study: unplanned refractive error and uveitis-glaucoma-hyphema syndrome. Intraocular lens exchange for unplanned refractive error typically took place within days of the primary surgery and was associated with the changing nature of cataract surgery, with patients and surgeons expecting specific refractive outcomes.
A uveitis-glaucoma-hyphema syndrome related to the increasing use of single-piece intraocular lenses with square-edged haptics was responsible for five intraocular lens exchanges in this study, all occurring after 2011. All five of these lenses were found to have been partially placed in the ciliary sulcus and were not exchanged until six to 15 years after primary cataract surgery. Study results were published in the American Journal of Ophthalmology in 2018.
"The population-based incidence of intraocular lens exchange has increased over the last three decades at a low and acceptable rate, but the overall increase in incidence was statistically significant," says Dr. Bothun. "The explanation may include increasing complications of primary cataract surgery or increasing surgeon comfort with exchanging lenses — a lower threshold for intervention. The major contributing factor, however, is likely to be the increase in the population at risk." The population-based incidence of cataract surgery doubled over the same period in Olmsted County.
Dr. Patel notes: "Surgeons should be aware of emerging indications of intraocular lens exchange, including unplanned refractive error and uveitis-glaucoma-hyphema syndrome from square-edged haptics in the ciliary sulcus, which reflect changes in lens design and increasing expectations of refractive outcomes."
For more information
Bothun ED, et al. Population-based incidence of intraocular lens exchange in Olmsted County, Minnesota. American Journal of Ophthalmology. 2018;187:80.
Rochester Epidemiology Project.