Nov. 12, 2024
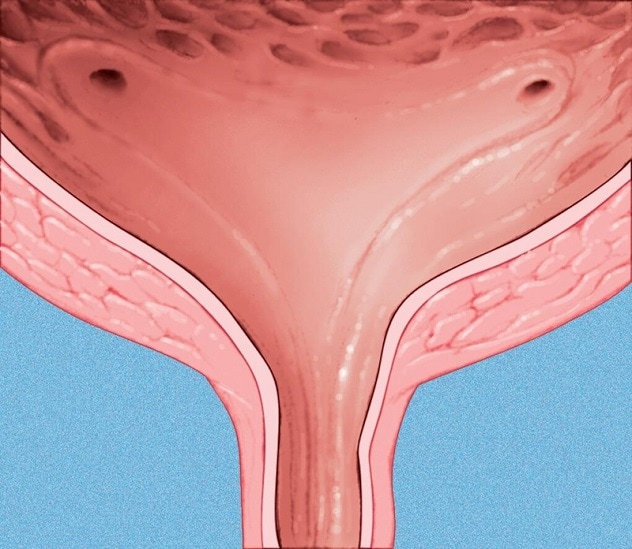 Incontinencia urinaria por esfuerzo
Incontinencia urinaria por esfuerzo
Incontinencia urinaria por esfuerzo
According to a 2024 American Journal of Obstetrics and Gynecology article by Mayo Clinic Obstetrics and Gynecology investigators, the definition of success for stress urinary incontinence (SUI) surgery depends on patients' perspectives.
The study found that patients' expectations for SUI success were lower than the stringent medical definition of success.
Consequently, when the Mayo Clinic investigators used a stringent definition of successful SUI surgery, what they considered success or failure often contradicted patients' own interpretations of successful treatment. A stringent definition would constitute complete dryness and a negative cough stress test result, which the study investigators found that patients did not consider necessary to deem the therapy successful.
Study aims and description
Emanuel C. Trabuco, M.D., a urogynecologist at Mayo Clinic in Minnesota, says he and fellow investigators wanted to determine, through this study, how to improve women's continence from their own perspectives. He notes that previous stringently performed, randomized clinical trials have found a 50% continence rate post-SUI surgery, yet satisfaction rates of 85% to 90%.
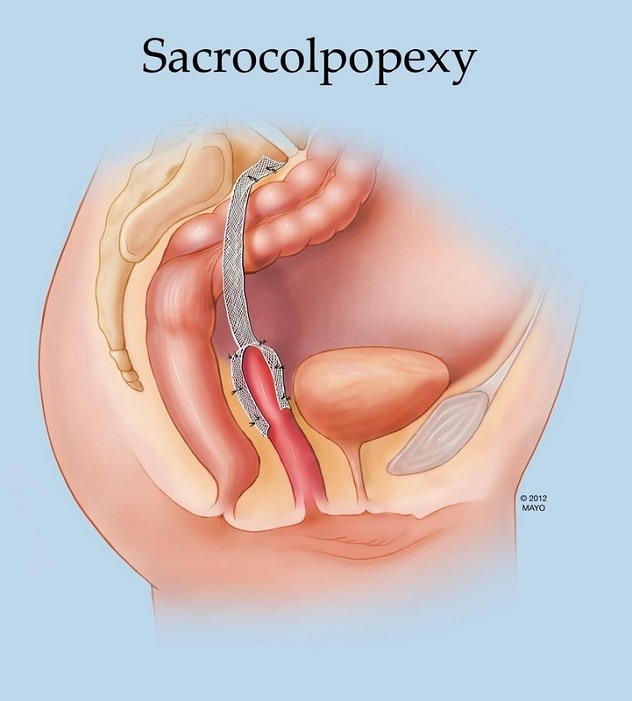 Sacrocolpopexia
Sacrocolpopexia
El tratamiento de la incontinencia urinaria por esfuerzo se puede realizar junto con la sacrocolpopexia, que es un procedimiento para reparar el prolapso.
To conduct this study, the investigators evaluated 51 different treatment success definitions for participants in a previous randomized SUI treatment trial. The current study involved treatments performed concurrently with sacrocolpopexy, a procedure to repair prolapse, in women with SUI. Between six and 24 months postsurgically, the investigators asked each study participant two questions about their SUI treatments:
- What is symptom improvement?
- What is your perception of surgical success?
Findings
The percentage of participants who had treatment success (6.4% to 97.3%) varied greatly according to each treatment success definition.
"The study simply showed that stringent definitions of continence do not correlate with patient perception of cure. Moreover, being completely dry, which we thought would be ideal, also was not considered optimal from the patients' perspective."
These questions led to an unexpected finding for the investigators: Women who were not leaking urine at all postsurgically were not as happy as women who leaked a little postsurgically.
"Our findings say that women tolerate a little leakage," says Dr. Trabuco. "Women were really satisfied if they had a small amount of leakage," he says. "Above that threshold of a little bit of leaking, women were not satisfied."
He indicates that some patients' perceptions of SUI treatment depended on where they started.
"Especially if the incontinence was bothersome enough at baseline, most patients were satisfied with a little bit of leakage postsurgically," says Dr. Trabuco.
He notes that women who appear to have had successful surgery could have other factors impacting their perceptions of success.
He adds that if patients underwent a cough stress test, their perception of success scores dropped by one-half. Dr. Trabuco finds this surprising since the cough stress test was previously considered an objective measure of continence.
"The study simply showed that stringent definitions of continence do not correlate with patient perception of cure," says Dr. Trabuco. "Moreover, being completely dry, which we thought would be ideal, also was not considered optimal from the patients' perspective. I hypothesize that this may be due to impact on bladder emptying."
Study applications to clinical care and future research
Dr. Trabuco says these findings do not significantly change his clinical consults at Mayo Clinic, although he indicates setting expectations with patients is critical with SUI surgery. He adds that having appropriate expectations is especially important if patients have more than one incontinence contributor. If a patient has an overactive bladder, for example, Dr. Trabuco indicates that SUI treatment is not necessarily going to fix that problem.
Beyond the clinic, this study's findings will affect Dr. Trabuco's research, especially in these ways, he says:
- He would not use the cough stress test.
- He would use less stringent definitions of surgical success with simple questionnaires that align with patient expectations.
Dr. Trabuco says one SUI research and treatment challenge is the lack of a gold standard test to diagnose SUI or SUI cure after surgery.
"Urodynamics is perceived as the gold standard SUI test, but it's not," he says. "It's neither sensitive nor specific, and we're using it before and after to measure SUI. If we could design an ambulatory test to measure what happens in real life, that would be ideal."
What really matters, according to Dr. Trabuco, is how patients are feeling and if they are no longer playing with their kids or running marathons like they used to due to SUI.
SUI referral to Mayo Clinic
An advantage of referring patients to Mayo Clinic for SUI is that Mayo urogynecologists perform SUI procedures frequently and have successfully completed thousands of SUI surgeries, according to Dr. Trabuco. He says that with this experience level, they know which patient characteristics are optimal for SUI surgery. The urogynecologists at Mayo Clinic also are well versed in consulting about surgical and nonsurgical options and are familiar with how to manage any complications that arise.
Dr. Trabuco says that Mayo Clinic urogynecologists are especially adept in situations in which previous surgery was unsuccessful or patients have mesh-related complications.
For more information
Trabuco EC, et al. Defining success after surgical treatment of stress urinary incontinence. American Journal of Obstetrics and Gynecology. 2024;231:235.e1.
Refer a patient to Mayo Clinic.