Nov. 12, 2024
A Mayo Clinic Reproductive Endocrinology and Infertility physician-scientist is striving for a better understanding of Asherman syndrome, which is rare, seeking to discover its cause and arrive at a standardized classification system. He also is pursuing in-depth multicenter research on treatment outcomes, especially regarding posttherapeutic healthy pregnancy potential.
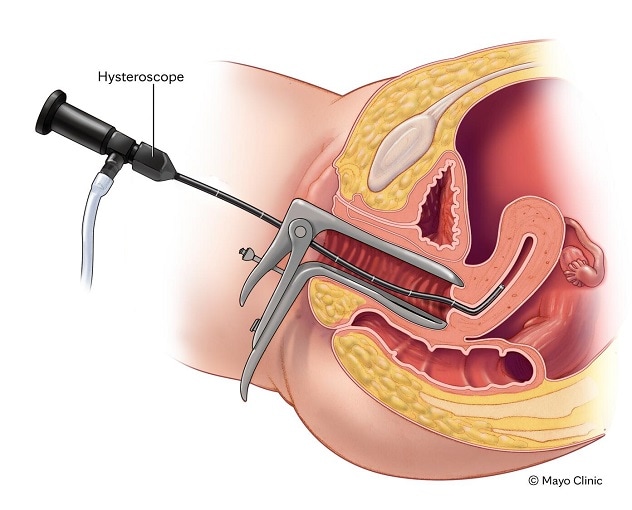 Síndrome de Asherman diagnosticado por histeroscopia
Síndrome de Asherman diagnosticado por histeroscopia
Un histeroscopio es un telescopio delgado con una luz que permite al médico observar la cavidad uterina. Se usa para diagnosticar el síndrome de Asherman.
Asherman syndrome involves intrauterine scar tissue that causes three key symptoms — infertility, menstrual abnormalities and pain — that are diagnosed via hysteroscopy. Zaraq Khan, M.B.B.S., a fertility specialist and minimally invasive gynecologic surgeon with expertise in Asherman syndrome at Mayo Clinic in Minnesota, says his interest in this syndrome peaked during his time as a Mayo Clinic scholar in the Netherlands working with Mark Hans Emanuel, M.D., Ph.D. Dr. Khan has continued to receive numerous patient referrals for serious Asherman syndrome during his time at Mayo Clinic. Mayo Clinic's Center for Regenerative Biotherapeutics also has funded his animal model research on this syndrome.
How Asherman syndrome arises and impacts patients
Though not life-threatening, Asherman syndrome has a significant quality-of-life impact on patients, most notably due to resulting infertility. However, patients with this diagnosis not seeking pregnancy or experiencing pain may live normal lives, says Dr. Khan.
Asherman syndrome diagnosis typically occurs postpartum following a miscarriage or live birth. For people who deliver and choose to breastfeed, menses often remain paused. However, those with Asherman syndrome may find themselves unable to become pregnant again, or their menses may not return or return abnormally, which can be confusing. For some, the disease process can start after a first or second trimester loss, but the highest risk of developing the disease tends to be postpartum, says Dr. Khan.
"Often when people who have Asherman syndrome are breastfeeding, they simply do not realize their menses aren't normal," says Dr. Khan. "They may know something's wrong, but they're not sure why."
The clinical pathway to an Asherman syndrome diagnosis may be winding but it can be more direct if patients see an OB-GYN specialist familiar with the syndrome and its symptoms.
Patients who experience Asherman syndrome typically are otherwise healthy, yet they have experienced pregnancy loss or infertility, says Dr. Khan.
Those who do not wish to have more children may be less concerned about the syndrome's symptoms than are those who desire additional children, he notes, and any pain may be treated with oral contraceptives. However, when Asherman syndrome leads to infertility for a couple, it can negatively affect both partners.
A syndrome with multiple unknowns
While medical professionals consider this syndrome rare, its degree of rarity is unknown: No reliable studies offer the true incidence, says Dr. Khan.
Asherman syndrome also presents other unsolved mysteries:
-
Etiology. The syndrome's causes remain unknown.
"Asherman syndrome is enigmatic — we don't know why scar tissue sets in," says Dr. Khan. "It's unusual that it develops in this location — the uterus. It appears to involve the perfect storm of infection, vigorous curettage and low estrogen levels."
Though uterine cavity scarring can occur due to infection, radiation or decreased blood flow to the organ following cauterization or other surgery, Dr. Khan says that true Asherman syndrome arises around pregnancy with trauma or insult to the gravid (pregnant) uterus. Instrumentation of the uterus in the form of a D&C at that time, either due to bleeding or a retained placenta, predisposes patients to scar tissue formation, says Dr. Khan. Factors leading to scar tissue development in these procedures remain a mystery, however.
"It's unfortunate the luck of the draw regarding when scar tissue will form following a procedure with the uterus," says Dr. Khan. "We don't yet know exactly what the triggering event in that procedure is."
-
Classification. No standard Asherman syndrome classification system exists. Three or four systems are used, says Dr. Khan, yet there is no agreement on which to use. This affects not only patient care but also the syndrome's investigation and potential therapy.
"Lack of a standardized classification system means it's hard to do global research because you're not comparing apples to apples," says Dr. Khan, mentioning that research involving a collaborative, multicenter team is the only efficient way to research a rare syndrome such as Asherman.
- Time to diagnosis. Dr. Khan says the average time to diagnosis for Asherman syndrome also remains unknown and requires more research.
- Successful posttherapeutic pregnancy. Existing research also does not provide an answer to the question of how many people undergo Asherman syndrome treatment and then experience successful pregnancy, says Dr. Khan. He reports anecdotally from his practice, however, that some patients go on to become pregnant and experience a live birth posttreatment.
Asherman syndrome treatment
Asherman syndrome treatment goals include:
- Scar tissue removal.
- Prevention of scar tissue recurrence.
- Healthy uterine lining restoration.
Hysteroscopic-guided adhesiolysis is the standard treatment for Asherman syndrome, including uterine cavity anatomical restoration. Whereas stem cells and platelet-rich plasma hold promise as uterine lining regenerative therapies, Dr. Khan says that currently, insufficient data exist to recommend these options. Investigation of optimal stem cell delivery and the most efficacious stem cells for Asherman therapy is still in its infancy.
While surgery can excise scar tissue and help restore the uterus, Asherman syndrome recurrence can plague patients, compelling them back to the OR two or three times for excision and uterine repair, says Dr. Khan. While Asherman specialists use several modalities to prevent a recurrence, he indicates that agreement on an optimal method remains elusive.
Asherman syndrome referrals
True Asherman syndrome medical centers are rare, says Dr. Khan, with 3 to 4 U.S. centers treating people with serious disease, including Mayo Clinic. He indicates that presently, little funding exists for the syndrome's research and there are few specialists.
Although this syndrome is rare, Mayo Clinic treats many patients with Asherman syndrome, which Dr. Khan considers advantageous for referring physicians.
"When things are rare, you want to have your patients go to a high-volume center," says Dr. Khan.
Mayo Clinic partners with local physicians to provide the full gamut of services to patients with Asherman syndrome. If surgical or nonsurgical treatments do not result in a desired pregnancy, Mayo Clinic also offers IVF and assistance connecting with a gestational carrier, who supplies the uterus for the pregnancy.
Dr. Khan suggests referring patients when a change in menstrual function or infertility is noted. He mentions, however, that this condition does not worsen if there is a delay.
"We are happy to collaborate with community physicians to help get to the bottom of a patient's challenges with pain, menstrual abnormalities or infertility," says Dr. Khan. "And we want to work with patients through Asherman syndrome therapy and any fertility treatment needed."
For more information
Refer a patient to Mayo Clinic.