May 26, 2023
Idiopathic normal-pressure hydrocephalus (iNPH) can be debilitating for people over age 60, yet it is underdiagnosed. Mayo Clinic is using cutting-edge technology to improve diagnosis and treatment approaches for this reversible condition.
"Right now, we're diagnosing this condition only in people with pretty severe symptoms, who may not get full recovery. We're hoping to pick up the diagnosis much sooner, so we can treat more patients."
The efforts involve sophisticated gait assessment, imaging and artificial intelligence. The goal is to better predict who might benefit from shunting.
"If the condition is caught early enough and patients undergo ventriculoperitoneal shunt placement, the symptoms can improve. Some individuals are even cured temporarily," says Olga P. Fermo, M.D., a neurologist and medical director of the cerebral spinal fluid (CSF) clinic at Mayo Clinic in Jacksonville, Florida.
Other efforts focus on improving surgical techniques. Mayo Clinic performs shunt placement laparoscopically. Research is also underway on technical innovations that could further reduce the invasiveness of shunt surgery.
"The surgery has stayed largely the same, with only minor variations, over the last 50 years. But we have had a lot of success with laparoscopic procedures," Dr. Elder says. "We end up with a much smaller incision and less risk of surgical complications, of the catheter being pulled out later, and probably also a lower risk of the catheter becoming obstructed."
Seeking diagnostic and prognostic markers
As many as 3% of individuals over age 60 might have iNPH. Untreated, the condition can cause gait disturbance, urinary incontinence and cognitive dysfunction. Diagnosis relies on a combination of clinical exam, MRI findings of ventricular dilation, CSF removal testing and gait assessment.
DESH
DESH
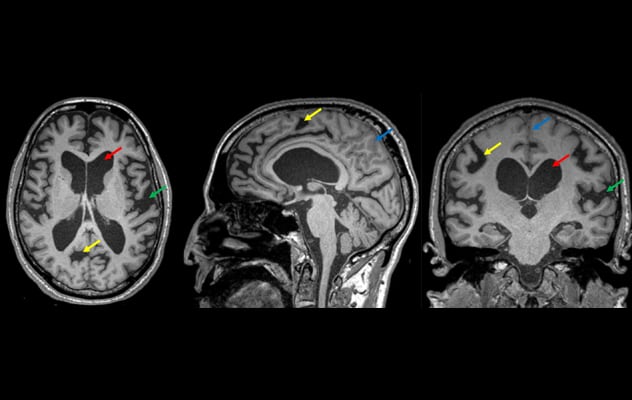
La resonancia magnética muestra rasgos de hidrocefalia con desproporción del espacio subaracnoideo en un individuo con hidrocefalia de presión normal idiopática. Las imágenes axiales, sagitales y coronales reformateadas de una secuencia 3D ponderada en T1 muestran ventriculomegalia (flechas rojas), estrechamiento y borramiento de los surcos en la línea media y el vértice (flechas azules) y agrandamiento de las cisuras de Silvio (flechas verdes). Los surcos con agrandamiento focal (flecha amarilla) están relacionados con trastornos en la dinámica del líquido cefalorraquídeo, lo que debe diferenciarse de la atrofia focal.
"We have developed a dedicated iNPH imaging protocol that provides multifaceted data and may help in diagnosis of challenging cases," says Petrice M. Cogswell, M.D., Ph.D., a neuroradiologist at Mayo Clinic's campus in Minnesota. "Increased awareness of imaging features associated with iNPH — specifically, disproportionately enlarged subarachnoid space hydrocephalus (DESH) — will help identify more individuals with this condition."
Comprehensive gait evaluations are performed before and after treatment. "The gait mat in our CSF clinic can record every aspect of gait and balance possible — step placement, step height and length, gait velocity, and stability," Dr. Fermo says.
Clinicians also collaborate with the Motion Analysis Laboratory at Mayo Clinic's campus in Minnesota. That teamwork between physicians and biomedical engineers facilitates optimal clinical decision-making and innovation.
"The lab provides highly detailed assessments of gait patterns to predict who might benefit from shunting. That information helps us to dial in the optimal shunt settings and to closely track improvements in walking over time," Dr. Elder says.
Mayo Clinic researchers are using gait assessment data to discern patterns associated with iNPH. The researchers also are applying artificial intelligence to pre-surgical and post-surgical imaging data to identify imaging markers of individuals who respond to shunt placement.
Other research efforts include:
- Analysis of genetic profiles of individuals with normal-pressure hydrocephalus.
- Participation in the multicenter Efficacy in iNPH Shunting (PENS) Trial, which is funded by the National Institute of Neurological Disorders and Stroke.
- Development of a test for axial movements in the horizontal position, as a potential prognostic indicator for shunt surgery.
- Investigation of the prognostic value of amyloid imaging before shunt surgery.
- Evaluation of the effectiveness of magnetic resonance elastography as an imaging modality for hydrocephalus.
- Characterization of serum and CSF biomarker profiles before and after shunt placement.
The scale of these efforts underlines Mayo Clinic's commitment to improving care for people with iNPH. Dr. Elder recalls two individuals he learned of during training who had symptoms of the condition. One was a 75-year-old marathon runner who was able only to jog occasionally. The other was a chief executive who had to retire due to inability to manage the business. Neither person had a diagnosis of iNPH after standard assessments.
"These individuals were clearly symptomatic of hydrocephalus, but our testing is too crude to pick up the subtleties of diagnosis," Dr. Elder says. "We diagnose only a small fraction of cases of a significantly debilitating condition. That has to improve."
For more information
Motion Analysis Laboratory. Mayo Clinic.
Efficacy in iNPH Shunting (PENS) Trial. ClinicalTrials.gov.
Refer a patient to Mayo Clinic.