Dec. 11, 2018
The clinical use of 7-Tesla MRI enhances Mayo Clinic's ability to manage epilepsy, certain brain and peripheral nerve tumors, and other neurological disorders. Mayo Clinic was the first center in North America to use clinical 7-Tesla MRI, after the Food and Drug Administration (FDA) approved the system in late 2017.
"The contrast and detail in particular clinical applications is exquisite," says Kimberly K. Amrami, M.D., a radiologist at Mayo Clinic in Rochester, Minnesota. "We're putting a lot of effort into developing usable, consistent protocols to apply this technology to a broad group of patients. Mayo Clinic's goal is to make 7-Tesla MRI a tool that will solve problems for our patients."
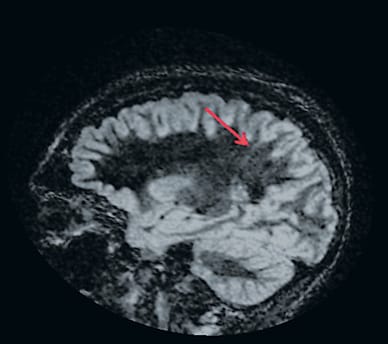
Displasia cortical focal en 7 Tesla

Displasia cortical focal en 7 Tesla
Las resonancias magnéticas de un paciente con epilepsia refractaria proporcionan una comparación de la calidad de imagen en 7 Tesla y en 3 Tesla. La displasia cortical focal (flecha) es más visible en esta imagen de 7 Tesla.
Displasia cortical focal en 3 Tesla
Displasia cortical focal en 3 Tesla
Las resonancias magnéticas de un paciente con epilepsia refractaria proporcionan una comparación de la calidad de imagen en 7 Tesla y en 3 Tesla. La displasia cortical focal (flecha) es menos visible en esta imagen de 3 Tesla.
The FDA approval covers clinical use of 7-Tesla MRI scans of the knee and brain. Mayo Clinic is using the system in selected patients to image peripheral nerves in the knee, to visualize tumors, microhemorrhages and multiple sclerosis (MS) lesions, and to locate seizure-origin sites in people with drug-resistant focal epilepsy. For that type of epilepsy, surgical resection is often curative when structural lesions are well-defined on MRI — but surgery is much less successful in patients with normal imaging.
"The 7-Tesla MRI has demonstrated its potential to uncover abnormalities that aren't detected using MRI with lower magnet strengths. Patients with drug-resistant focal epilepsy who have a normal 1.5-Tesla or 3-Tesla MRI and who are considering surgical resection should have a 7-Tesla MRI," says Gregory A. Worrell, M.D., Ph.D., a neurologist at Mayo Clinic's campus in Minnesota. "The 7-Tesla MRI might also benefit patients who are being considered for the implantation of intracranial electrodes for brain stimulation."
Defining characteristics
The 7-Tesla MRI provides enhanced detail in cortical imaging, reducing blurring between gray and white matter. "Since the signal to noise ratio is more than doubled, what is invisible or a little ambiguous in a 3-Tesla MRI can be much more clearly defined on the 7-Tesla system," Dr. Amrami says.
As a result, small MS plaques and their relationship to cerebral veins are more clearly visible on 7-Tesla MRI, facilitating earlier diagnosis. In addition, the stronger magnetic field enhances the prominence of magnetic susceptibility effects, which can be useful in the diagnosis of tiny intracranial bleeds or other diseases of cerebral blood vessels.
"With the 7-Tesla MRI, we can detect subtle traumatic brain injury or tiny hemorrhages caused by hypertension or amyloid angiopathy that would be difficult or impossible to see on other scanners," says Kirk M. Welker, M.D., a neuroradiologist at Mayo Clinic's campus in Minnesota.
Functional MRI is similarly enhanced. "Detecting small changes in brain blood flow is much easier at 7 Tesla and allows us to generate more-accurate functional maps to avoid injuring critical brain areas during tumor removal or seizure surgery," Dr. Welker says.
When used to image the knee, 7-Tesla MRI can guide decision-making for peripheral nerve surgery. "At 7-Tesla strength, we can start to see individual nerve bundles, which is very useful if a problem doesn't affect an entire nerve," Dr. Amrami says. "When a cyst is associated with the nerve coming from the knee or superior tibiofibular joint, we can actually see the joint connection and the tiny nerve that innervates the joint much better than at 3 Tesla."
The 7-Tesla system is less suitable for imaging certain structures near the skull base, such as the inferior temporal lobes, pituitary gland or internal auditory canal. "Bone and air in the skull base cause a greater degree of imaging artifact at 7 Tesla than at lower field strengths," Dr. Welker says. "Our medical physicists are investigating potential solutions to these problems so they may be less of a concern in the future." In addition, safety constraints for implanted metal objects in the body are much greater for 7-Tesla MRI.
A leader in neuroimaging
Mayo Clinic has a distinguished history of imaging. In 1973, Mayo Clinic was the first center in North America to use CT. Mayo was an early adopter of MRI and the first center in the United States to use clinical 3-Tesla MRI, as well as a leader in the use of positron emission tomography.
"We're now exploring ways to expand our use of 7 Tesla to improve patient care," Dr. Amrami says. "The 7-Tesla system is unique among our 40 MRI scanners, and provides us with an exciting new set of capabilities for diagnosing disease. We're actively working to learn which groups of patients stand to benefit the most from a 7-Tesla scan."