Aug. 22, 2024
Total abdominal proctocolectomy with ileal pouch-anal anastomosis (IPAA) for ulcerative colitis (UC) is the restorative procedure of choice for patients with medically refractory UC and patients with UC-related neoplasia. Also known as a J-pouch procedure, this surgery preserves the anal sphincter and fecal continence, and it eliminates the need for an external ostomy afterward.
J-pouch surgery is associated with high patient satisfaction and good functional outcomes in many patients. However, related complications include structural and inflammatory pouch disorders, and pouch failure followed by pouch excision or permanent diversion.
In a review article published in the American Journal of Gastroenterology in 2024, Mayo Clinic researchers provided an overview of the most common inflammatory and structural disorders of the pouch, and they summarized recent research findings related to their evaluation and management.
In this Q&A, Laura E. Raffals, M.D., highlights some of the information presented in that review article. Dr. Raffals, the corresponding author on the review article publication, is a gastroenterologist and a member of the Inflammatory Bowel Disease Clinic at Mayo Clinic in Rochester, Minnesota.
Why is gaining a better understanding of J-pouch disorders an important topic right now?
The prevalence of inflammatory bowel disease is rising, which means there are more patients living with J-pouch than ever before. However, we lack reliable risk stratification tools and guidelines outlining approved, effective therapies for the management of patients with pouch inflammation.
What types of pouch disorders can occur, and what is the most common form?
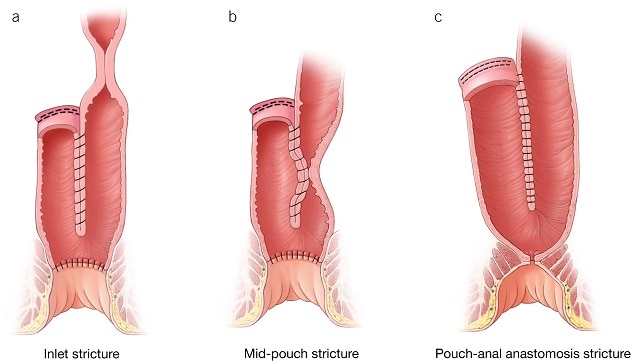 Trastornos estructurales de la bolsa: constricciones
Trastornos estructurales de la bolsa: constricciones
A menudo observadas después de una anastomosis manual, las constricciones suelen estar ubicadas normalmente en (a) la entrada de la bolsa, (b) la parte media de la bolsa y (c) la anastomosis ileoanal.
J-pouch disorders can be divided into two categories — inflammatory pouch disorders and structural pouch disorders. Pouchitis is the most commonly occurring disorder, affecting an estimated 40% of patients undergoing J-pouch surgery within the first year after the procedure. Some patients develop chronic inflammation of the pouch that may or may not respond to antibiotic therapy. This complication was the focus of the EARNEST trial — the first large randomized clinical trial for chronic pouchitis. Our article describes the major categories of pouch disorders in detail, listed in a table here.
What are some of the tools available to evaluate these disorders?
Our article provides an overview of the multiple endoscopic, imaging and scoring tools used in the evaluation of pouch disorders. To summarize, we can use pouchoscopy to document the extent and nature of inflammation, identify pouch complications and structural disorders, and perform surveillance of dysplasia and neoplasia.
Abdominal and pelvic imaging, including computerized tomography enterography and magnetic resonance enterography, can help identify strictures, abscesses and inflammation extent in the pouch and small bowel. Pelvic magnetic resonance imaging is useful for identifying structural complications, fistulas involving the pouch and anal transition zone, and length of rectal cuff.
Functional testing — including the use of barium and magnetic resonance defecography and anorectal manometry and balloon expulsion — can facilitate dynamic evaluation of pouch function and evacuation disorders. Finally, we have several scoring systems that can help determine pouchitis indexes, including the Pouchitis Disease Activity Index (PDAI) and modified PDAI and the Chicago Classification of Pouchitis.
What can you tell us about the management options available to manage pouch disorders?
Therapies for inflammatory pouch disorders include antibiotics, biologics, biologics in combination with immunomodulators and steroids, and procedures to address fibrostenotic or penetrating disease. Tools for managing structural pouch disorders include behavioral management (for floppy pouch complex) and a variety of pharmacologic therapies and endoscopic and surgical procedures. Advances in endoscopic therapies and minimally invasive surgery techniques are providing additional options for managing these disorders. Our article provides a detailed review of available management options and data related to their efficacy.
What additional research is needed to further advance our knowledge about pouch disorders?
Additional studies are needed to develop our understanding of the pathophysiology of pouchitis, and the importance of achieving endoscopic healing in patients with pouch inflammatory disorders. We need to learn whether we should treat to target mucosal healing in pouches, similar to how we approach Crohn's disease and ulcerative colitis. It is particularly important to understand if it is OK to recycle advanced therapies previously tried in patients before they undergo a colectomy, as so many of our patients are now treated with multiple advanced therapies prior to colectomy. I anticipate that large pragmatic trials comparing different treatment strategies are where the field will be headed next.
For more information
Santiago P, et al. Classification and management of disorders of the J pouch. American Journal of Gastroenterology. 2023;118:1931.
Refer a patient to Mayo Clinic.