Dec. 21, 2024
Kenton R. Kaufman, Ph.D., director of the Motion Analysis Laboratory at Mayo Clinic in Minnesota, believes strongly that a laboratory setting is not always the right environment to monitor a patient's function before or after treatment.
"We need real-world evidence of patient outcomes," he says. "In a natural environment, nobody's walking to impress the doctor."
Two key goals of wearable sensors, says Dr. Kaufman, are:
- Provide objective outcome data in the free-living environment.
- Provide a tool for physicians to monitor patients and provide objective, reliable data to guide treatment.
Dr. Kaufman sees this as a collaborative process — versus a correctional or parental one — in which the patient and the physician work together on goal setting.
"It's not punitive — it's collaborative," he says.
Dr. Kaufman says the most common method of quantifying a patient's outcome in orthopedics is asking the patient to complete a questionnaire. Although he says questionnaires still have a place in obtaining information about a patient's quality of life, they do not provide the same data quality as sensors.
Dr. Kaufman's laboratory work with sensors
In the Motion Analysis Laboratory, Dr. Kaufman and his staff have conducted many scientific studies with wearable sensors, including algorithm development, validation and optimization.
Around 2010, wearable sensors became a major focus in his laboratory when a medical device company contacted Dr. Kaufman to offer expertise on a new prosthetic. The company spent an entire morning showing Dr. Kaufman all the features of this new device in a patient model. However, when Dr. Kaufman went to lunch with the company representatives and the patient, Dr. Kaufman noticed that the patient used none of the prosthetic's features.
This observation of the patient's behavior with the prosthetic led Dr. Kaufman and his laboratory to develop software algorithms to understand what patients were doing during the day, such as:
- Activity: lying down, sitting, standing or running.
- Inactivity: sedentary bouts and breaks.
He notes that these algorithms are useful for studying a wide variety of patients with orthopedic conditions, including those who have hip, knee or shoulder replacement, scoliosis surgery, or amputation.
More recently, Dr. Kaufman's lab has collaborated with a company to validate a sensor capable of collecting data for up to 6 months and displaying the patient's daily activity in an app for the patient and physician.
"A partnership between the patient and the physician is everything. A wearable sensor gives the complete picture of the patient's daily reality so that the most optimal outcome can be achieved."
U.S. healthcare environment changes affect remote therapeutic monitoring reimbursement
Dr. Kaufman indicates that the healthcare environment is changing to value-based care, as described in a 2006 book published by Harvard Business School Press, and this has impacted the field of remote therapeutic monitoring and its reimbursement.
"In this scenario, achieving optimal patient outcomes at a lower cost to the patient and payer is the primary goal," he says.
Furthering the emphasis on value-based care, the Institute for Healthcare Improvement communicated its Triple Aim of a value-based care framework in 2008:
- Improve the patient experience of care, including quality and satisfaction.
- Improve the health of the population.
- Reduce the per capita cost of healthcare.
Dr. Kaufman says that to achieve these aims, the Centers for Medicare & Medicaid Services has recently approved remote therapeutic monitoring codes to collect and monitor nonphysiologic patient data related to therapeutic interventions.
Another key shift in the U.S. healthcare environment is that the Food and Drug Administration now requests real-world evidence for therapeutic product development.
Benefits of remote therapeutic monitoring for physicians
 Physician dashboards
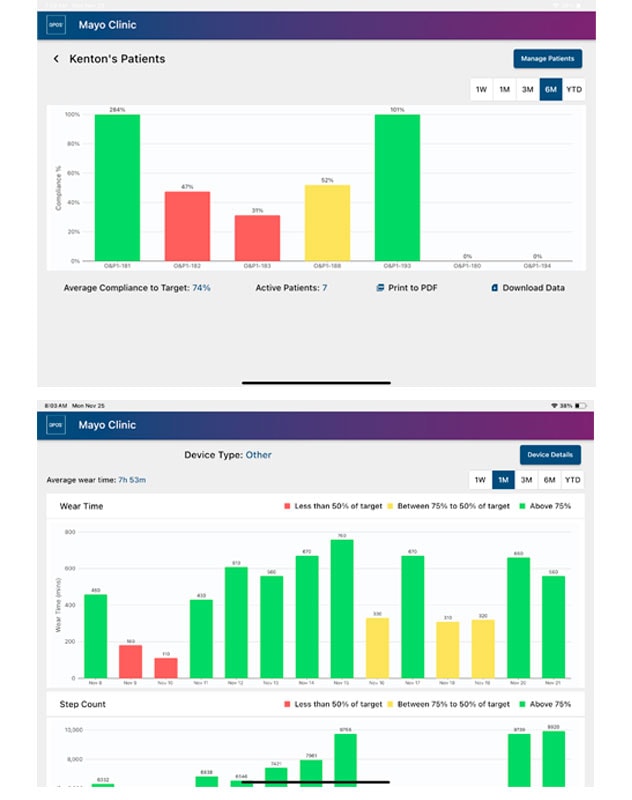
Physician dashboards
These wearable sensor physician dashboards show multiple patients (top) and a single patient's daily record (bottom). All patients are de-identified.
Dr. Kaufman sees a variety of positives for physicians who offer remote therapeutic monitoring to their patients receiving orthopedic care:
- Joint physician-patient goal setting. The physician and patient can set therapeutic goals together, such as wearing a brace or being active for a given number of hours a day.
- Adherence. Physicians can monitor patient adherence to a treatment plan. Remote therapeutic monitoring provides reliable data on the patient's activity instead of dialogue at an appointment following surgery or other treatment.
- Reimbursement. There is a CPT code for this monitoring. Medicare reimburses physicians for this service.
"A partnership between the patient and the physician is everything," says Dr. Kaufman. "You cannot get a good outcome for a patient without adherence to the treatment plan. A wearable sensor gives the complete picture of the patient's daily reality so that the most optimal outcome can be achieved."
How patients respond to remote therapeutic monitoring
Patients respond positively to the use of a wearable sensor and the data it provides. Sensors allow patients to observe progress on established posttreatment goals in real time and determine if they are on track for optimal recovery.
"Use of remote monitoring can lead to better outcomes faster due to the regularly provided feedback, which allows for adjustments," he says.
Dr. Kaufman describes the remote therapeutic monitoring experience as completely unlike having an Orwellian Big Brother watching. These devices have no GPS. The wearable sensors can tell physicians if the patient is wearing a device prescribed postsurgically and if the patient is active, but not where the patient is located.
Sensor accessibility
Dr. Kaufman says that sensors are typically inexpensive for patients and their insurers, and some are designed to be disposable.
He also says that wearable sensors are readily available to physicians and their patients in their communities.
For more information
Motion Analysis Laboratory: Kenton R. Kaufman. Mayo Clinic.
Porter ME, et al. Redefining Health Care: Creating Value-Based Competition on Results. Harvard Business School Press; 2006.
Triple aim and population health. Institute for Healthcare Improvement.
Real-world evidence. U.S. Food and Drug Administration.
Refer a patient to Mayo Clinic Orthopedics and Sports Medicine in Minneapolis.