March 31, 2023
Although pancreatic cancer accounts for only 3% of new cancer diagnoses, it is projected to become the second most common cause of cancer-related death in the United States by 2030, according to the National Cancer Institute. Surgery is the only known cure for patients without obvious metastases. Patients whose tumors involve critical blood vessels, also called borderline resectable or locally advanced, are often treated with neoadjuvant therapy including systemic chemotherapy followed by consolidative chemoradiation, with some patients being considered for complex surgical resection afterward.
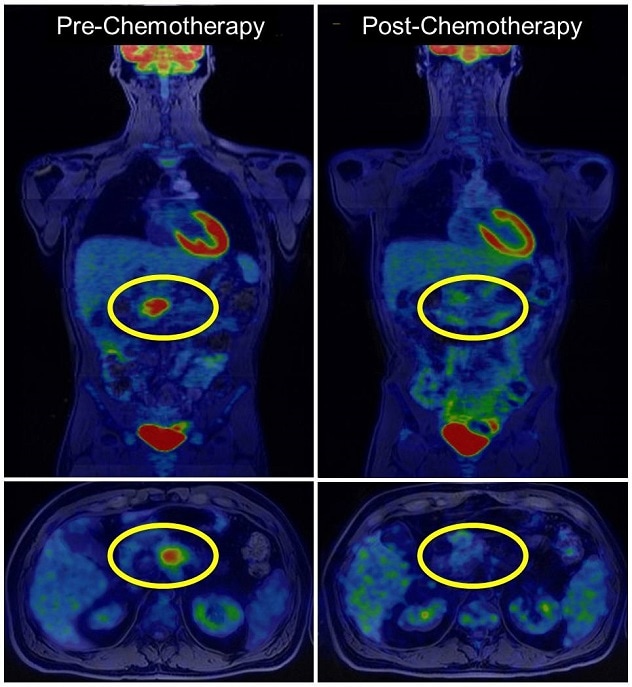
Traditional cross-sectional imaging such as CT and MRI poorly predicts response to this neoadjuvant therapy, and National Comprehensive Cancer Network guidelines don't currently include radiologic response as a metric. PET imaging has been used in many other types of cancer but is not typically used for patients with pancreatic cancer.
Although a blood-based tumor marker, CA 19-9, does exist to monitor the impact of neoadjuvant therapy, it has limited sensitivity. Furthermore, 10% of patients do not have measurable levels, called nonsecretors, and up to one-third of patients present with normal levels of CA 19-9. For the 60% of patients who would exhibit a CA 19-9 level useful to their care plans, there is disagreement in the field about the optimal decrease of that marker to indicate the best possible surgical outcomes.
Physicians at Mayo Clinic, however, have been using FDG-PET imaging to measure treatment response and predict surgical outcomes for several years to address this unmet need.
"The PET scan adds to all the different things we monitor to help patients make the most informed decisions," says Mark J. Truty, M.D., M.S., a surgical oncologist at Mayo Clinic Comprehensive Cancer Center in Rochester, Minnesota.
A retrospective analysis of Dr. Truty and his colleagues' use of PET imaging for patients with pancreatic cancer was published in the Journal of the National Comprehensive Cancer Network in September 2022. This research has the potential to change treatment response guidelines for all patients with pancreatic cancer throughout the country.
Retrospective review of PET imaging cohort
Exploración por tomografía por emisión de positrones para detectar cáncer de páncreas
Exploración por tomografía por emisión de positrones para detectar cáncer de páncreas
La tomografía por emisión de positrones (PET, por sus siglas en inglés) muestra lesiones pancreáticas antes y después de la quimioterapia.
The final cohort reviewed included 202 patients with a mean age of 64.7 years at the time of surgery. Women accounted for 42% of the cohort. All patients received first line neoadjuvant chemotherapy, and 94 patients underwent chemotherapy switch. Nearly all patients (91%) had preoperative chemoradiation following neoadjuvant therapy.
Of the initial cohort, 46 patients had normal CA 19-9 levels at diagnosis and 21 patients were nonsecretors. Only 67% of patients presented with an elevated CA 19-9 level at diagnosis, and half of those patients' levels had normalized following neoadjuvant therapy.
All patients had at least one FDG-PET scan following neoadjuvant therapy and before surgical resection, and 90.1% of patients had two or more.
PET imaging results correlate with surgical outcomes
There is a significant association between neoadjuvant therapy pathologic response and patient survival. However, researchers only know the results of pathologic response after surgery. Dr. Truty and his colleagues assessed preoperative factors using biochemical response measured with CA 19-9 level and metabolic response measured with FDG-PET. Both were compared with neoadjuvant pathologic response.
Major pathologic response was more likely in patients with optimal CA 19-9 levels, major CA 19-9 response and major metabolic response. Without the presence of major metabolic response, biochemical response did not correlate with major pathologic response. On the contrary, major metabolic response was highly associated with major pathologic response regardless of biochemical response. When both biochemical and metabolic factors were observed, pathologic response was even more predictive.
"The most rewarding part of this is that we are able to have more-informed discussions with our patients," said Ajit H. Goenka, M.D., a radiologist with Mayo Clinic Comprehensive Cancer Center in Rochester, Minnesota. "We can have shared decision-making with them."
The future of pancreatic cancer care
Drs. Truty and Goenka developed this concept in a true testament to Mayo Clinic's multidisciplinary model of care.
"It all started as a hallway conversation," says Dr. Goenka. "We have this cross-pollination of ideas and thoughts about problems. The culture of Mayo Clinic helps people from different disciplines come together to solve problems."
Research is underway to evaluate new imaging tracers. In the meantime, FDG-PET imaging is something all practitioners can do for their patients with pancreatic cancer.
"We can actually consider taking patients to the operating room for more-complex operations because we can highly predict whether or not they received effective chemotherapy, and we can change things if the chemotherapy isn't effective," says Dr. Truty. "The real future is not just to make sure that there are better drugs but also to prove the drugs we're giving are beneficial."
Dr. Truty, Dr. Goenka and their colleagues in the field discussed this research and other pancreatic cancer care optimizations in a webinar in December 2022.
For more information
Annual report to the nation 2022: Overall cancer statistics. National Cancer Institute.
Abdelrahman AM, et al. FDG-PET predicts neoadjuvant therapy response and survival in borderline resectable/locally advanced pancreatic adenocarcinoma. Journal of the National Comprehensive Cancer Network. 2022;20:1023.
Refer a patient to Mayo Clinic.